Int J Drug Res Clin. 2:e7.
doi: 10.34172/ijdrc.2024.e7
Original Article
Ultrasonography Findings in Post-Methotrexate Treatment of Cesarean Scar Pregnancy
Elham Eghbali 1, *  , Mahsa Karbasi 1, Maryam Sodabi 1, Esmaeil Farhadi 1, Ali Nikoukhesal 1, Nima Ghanini 1, Alireza Omara Shahestan 1, Fatemeh Abbasalizadeh 2, Farzad Razmifard 3
, Mahsa Karbasi 1, Maryam Sodabi 1, Esmaeil Farhadi 1, Ali Nikoukhesal 1, Nima Ghanini 1, Alireza Omara Shahestan 1, Fatemeh Abbasalizadeh 2, Farzad Razmifard 3
Author information:
1Medical Radiation Sciences Research Group, Tabriz University of Medical Sciences, Tabriz, Iran
2Department of Obstetrics and Gynecology, Tabriz University of Medical Sciences, Tabriz, Iran
3Faculty of Nutrition and Food Sciences, Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran
Abstract
Background:
Cesarean scar pregnancy (CSP) can cause life-threatening complications for pregnant women, so early diagnosis and treatment are crucial for the prevention of maternal mortality. Transvaginal color Doppler ultrasonography, along with serum beta-human chorionic gonadotropin (β-hCG) level follow-up, can be a noninvasive and proper method for the post-treatment follow-up of a CSP. The present study investigated the Doppler resistance index (RI) changes in CSPs after medical management with methotrexate (MTX), evaluated by sac diameter and serum β-hCG level measurement.
Methods:
Overall, 28 patients with CSP and a history of previous cesarean delivery, a gestational age of less than 9 completed weeks at ultrasonography, the decision to medical management by the gynecologist, and having a β-hCG level before treatment were enrolled and initially examined by ultrasound and Doppler studies. The RI of the closest myometrial artery to the CSP mass and its diameter underwent measurement. After 72 hours, 1 week, and 2 weeks of medical therapy with MTX, the mentioned variables were measured again and compared with the values of the pretreatment time point.
Results:
RI values were significantly higher at all the follow-up time points compared with the pre-treatment time points, while serum β-hCG levels were significantly lower. Moreover, sac diameter values increased 72 hours post-treatment and then represented a decline.
Conclusion:
Serial Doppler ultrasound examination can be a useful method to evaluate the success or failure of the medical management of CSPs, as the increase in RI values occurs rapidly after medical treatment and correlates well with serum β-hCG levels.
Keywords: Cesarean scar pregnancy, Medical management, Resistance index, Transvaginal color doppler ultrasonography
Copyright and License Information
© 2024 The Author(s).
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
None.
Please cite this article as follows: Eghbali E, Karbasi M, Sodabi M, Farhadi E, Nikoukhesal A, Ghanini N, et al. Ultrasonography findings in post-methotrexate treatment of cesarean scar pregnancy. Int J Drug Res Clin. 2024; 2: e7. doi: 10.34172/ijdrc.2024.e7
Introduction
Cesarean scar pregnancy (CSP) occurs when a gestational sac implants at the site of a previous cesarean section scar.1 CSP is extremely rare, with an estimated incidence of 1 in 1800 to 1 in 2500 pregnancies.2,3 However, the occurrence of CSP has increased due to the notable rise in the rates of cesarean deliveries (CD) and the development of imaging tools such as transvaginal ultrasonography (TVUS).4 Vaginal bleeding with or without lower abdominal pain is the most common clinical manifestation of a CSP.5 However, almost one-third of incidentally diagnosed CSPs are asymptomatic.6,7 Life-threatening complications, including placental abnormalities such as accreta, massive hemorrhage, and uterine rupture, may occur if CSP is not diagnosed timely and allowed to progress.2 Thus, the early diagnosis and management of CSPs are vital. Any pregnant woman with a prior history of CD should be scanned for a CSP with TVUS and with transvaginal color Doppler ultrasonography (TVCDUS) to detect the site of the gestational sac as soon as possible during the first trimester.5,8
The management strategy of a CSP may differ individually. Expectant management, medical treatment, various surgical approaches, or a combination of these may be taken into consideration 9. Nevertheless, there are few standardized guidelines for CSP management.
Checking serum beta-human chorionic gonadotropin (β-hCG) levels is commonly used for the post-treatment follow-up of a CSP. However, it has been shown to have some restrictions, such as not providing any information on the blood flow of the mass.10 Therefore, some studies have suggested serial Doppler ultrasound examinations for a CSP post-treatment follow-up, together with the serum β-hCG measurement.11 This study aimed to investigate the Doppler resistance index (RI) changes in CSPs after medical management, along with sac diameter and serum β-hCG level measurement.
Methods
This cross-sectional study was conducted at the Department of Radiology, Al-Zahra hospital of Tabriz Medical University, Iran, from January 2021 to June 2022. In general, 30 patients with CSP were enrolled in the study after approval by the Ethics Committee of Tabriz University of Medical Sciences. The inclusion criteria were having a history of previous CD, a CSP report with a gestational age of less than 9 completed weeks at ultrasonography, decision for medical management by a gynecologist, and having a β-hCG level before treatment. On the other hand, the decision for surgical management by the gynecologist, the lack of a serum β-hCG level before treatment, and the lack of consent to be included in the study were the exclusion criteria.
The patients included in the study were initially examined by TVUS and TVCDUS. The RI of the closest myometrial artery to CSP mass, CSP mass diameter, and the pretreatment β-hCG level were measured and recorded. Patients with non-viable embryos and a β-hCG level of less than 5000 mIU/mL were treated with a single dose of 50 mg systemic methotrexate (MTX), and those with a beta-hCG level of more than 5000 mIU/mL were treated by an intragestational (intrasaccular) injection of 25 mg of MTX in addition to the single dose of systemic MTX. Moreover, CSPs with fetal heartbeats were treated by an injection of 8 mEq intrasaccular potassium chloride in addition to the single dose of systemic MTX. The mentioned variables were measured and recorded after 72 hours, 1 week, and 2 weeks of medical management and compared with the values of the previous time point. All the TVS and color Doppler ultrasound examinations were performed by a radiologist with proper experience in obstetrics ultrasound using a Philips Affiniti 70 ultrasound device, a convex ultrasound probe with a frequency range of 2‒5 MHz, and a 4‒7 MHz vaginal probe. Several traces were taken in all the color Doppler evaluations, and RI was measured and recorded. Serum β-hCG levels were obtained by an enzyme-linked immunosorbent assay. The patients were included in the study after giving their written informed consent.
Numerical data were calculated and presented as means (SD) or medians (IQR) based on their shape of distribution. P values for comparing RI and sac diameter at each time with the values of previous time points were calculated by the parametric test of repeated measures analysis of variance, and paired comparisons were performed using Bonferroni adjustment. In addition, the Friedman non-parametric test was used for calculating P values utilized for comparing β-hCG levels before and after treatment time points, and the Dunn adjustment was employed for paired comparisons. GraphPad Prism (version 9) was applied for statistical analysis, and a P value of more than 0.05 was considered significant.
Results
Based on the inclusion and exclusion criteria, 28 cases were included in the study, and 2 cases were excluded due to medical treatment failure and a decision for surgical treatment. Demographic and obstetric characteristics of the studied cases are presented in Table 1. Of the 28 cases before the treatment, 5 (17.86%) were diagnosed with fetal heartbeats. Seventy-two hours after the treatment, no heartbeats were detected in the ultrasonography.
Table 1.
Baseline Characteristics of Patients
|
Variable
|
Mean (SD)
|
Minimum
(wk)
|
Maximum
(wk)
|
| Maternal age |
31.53 (3.76) |
25 |
41 |
| Gestational age (wk) |
5.57 (0.69) |
5 wk + 1 d |
8 wk + 3 d |
| Pregnancy frequency |
2.71 (1.05) |
2 |
7 |
| CD frequency |
1.68 (0.86) |
1 |
4 |
| The interval between the last CD and the current CSP (y) |
4.10 (1.89) |
2 |
9 |
Note. SD: Standard deviation; CD: Cesarean delivery; CSP: Cesarean scar pregnancy.
The data analysis demonstrated that RI values were significantly higher at all the follow-up time points compared with the previous time point, while serum β-hCG levels were significantly lower (Figure 1, Table 2). Moreover, sac diameter values increased 72 hours post-treatment, then represented a reduction.
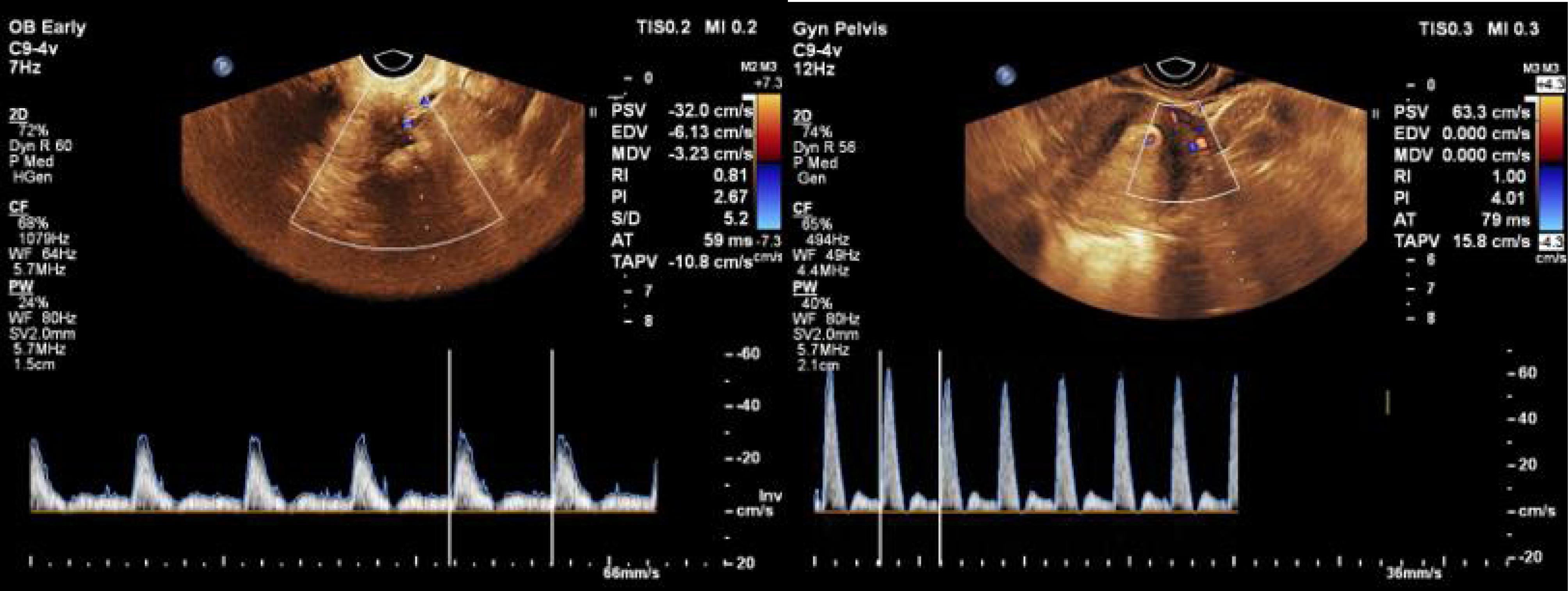
Figure 1.
RI Measurement From the Closest Myometrial Artery Adjacent to the CSP Before (a) and After (b) Treatment. Note. RI: Resistive index; CSP: Cesarean scar pregnancy. The results show an increase in the amount of RI from 0.81 to 1 following medical treatment
.
RI Measurement From the Closest Myometrial Artery Adjacent to the CSP Before (a) and After (b) Treatment. Note. RI: Resistive index; CSP: Cesarean scar pregnancy. The results show an increase in the amount of RI from 0.81 to 1 following medical treatment
Table 2.
Laboratory and Imaging Parameters Before and After Medical Treatment of CSP
|
Time
|
RI
|
Sac Diameter (mm)
|
Serum β-hCG (mIU/mL)
|
|
Mean (SD)/
P
Value
|
Mean (SD)/
P
Value
|
Median (Q1-Q3)/
P
value
|
| Before treatment |
0.47 (0.11) |
37 (22) |
9800 (2788-10225) |
| Seventy-two hours after treatment |
0.59 (0.11) / < 0.0001 |
42 (17) / 0.48 |
4660 (1300-81175) / < 0.05 |
| One week after treatment |
0.69 (0.11) / < 0.0001 |
33 (11) / 0.0003 |
1082 (470-1900) / < 0.05 |
| Two weeks after treatment |
0.82 (0.12) / < 0.0001 |
27 (10)/ < 0.0001 |
345 (223-588) / < 0.05 |
Note. RI: Resistance index; SD: Standard deviation; mm: Milli meter; β-hCG: Neta human chorionic gonadotropin; CSP: Cesarean scar pregnancy.
Discussion
CSP is a very rare type of ectopic pregnancy with life-threatening complications,12 accounting for 6.1% of ectopic pregnancies among women with a previous history of CD.2,13 Recently, there has been a rise in CSP rates due to the considerably elevated number of CDs worldwide.14 Therefore, early diagnosis and effective management and follow-up of CSP are crucial. The exact etiology of this condition remains unknown. A small defect in the uterine incision due to poor healing of the injuries caused by CDs, several uterine curettages, and adenomyosis are some of the proposed possible mechanisms of CSP development. Further, multiple risk factors such as the number of previous cesarean sections, the interval between the prior CD and the next pregnancy, the indications for the previous cesarean sections, and the surgery technique have been suggested, though the correlation between these factors and CSP has not been proved yet.15 Delays in the diagnosis and treatment of patients with CSP may be associated with a high risk of uterine rupture, massive hemorrhage, hysterectomy, fertility loss, and maternal mortality.16-18 The diagnosis of CSP is usually difficult, and the reported rate of misdiagnosis is significant.19 Ultrasonography is the first-line imaging modality for CSP diagnosis.20 Recent progress in transvaginal and three-dimensional ultrasonography has led to earlier diagnosis and more effective management of CSP to prevent its catastrophic complications.21 Moreover, it has been indicated that color Doppler imaging may be highly useful in the early and accurate detection of CSPs.22
Due to the rarity of CSP, there has been no consensus on the optimal management strategy of CSP.5,20 A variety of treatment options, including expectant management, medical treatment programs, and multiple surgical interventions, have been described in the literature.5 In most cases, a combination of these methods has been used to eliminate these ectopic embryos.2 Selecting the most appropriate treatment approach depends on the patient’s clinical features, gestational age, size of the mass, serum β-hCG levels, and the clinical experience of the physician.8
Although there are no guidelines for optimal follow-up methods after the medical management of a CSP, the serum β-hCG level has been shown to be a suitable marker.14 However, serum β-hCG levels provide no information on the blood flow of the mass.23 Moreover, some cases have reported that despite the excessive drop (even to normal values) in β-hCG levels after medical therapy, the mass did not resolve, resulting in serious consequences.8,24 In these cases, it has been suggested that serial transvaginal Doppler ultrasound examinations may be helpful for investigating medical management success.11
The data obtained from the present study revealed that serum β-hCG levels decreased significantly after medical treatment at each time point compared with the previous time point and the baseline (before the treatment) levels, while the RI values of Doppler ultrasound increased significantly. In a study on the evaluation of the efficacy of high-intensity focused ultrasound in the treatment of cesarean section scar pregnancies, Huo et al observed that RI values were significantly elevated four weeks after the treatment, while blood β-hCG levels significantly decreased compared with their pretreatment values.23 These findings are compatible with our results, although there are some differences in the methods of treatment and follow-up between the two studies.
The number of previous studies evaluating the changes in color Doppler findings in CSP after treatment with MTX is rare. Shi et al investigated the diagnostic value of transvaginal three-dimensional ultrasound (3D-US) combined with color Doppler ultrasound for early CSP diagnosis. They concluded that the diagnostic accuracy of transvaginal 3D-US combined with color Doppler US was significantly higher than that of transvaginal 3D-US. It was further found that transvaginal 3D-US combined with color Doppler US can improve the sensitivity, specificity, and accuracy of the diagnosis of early CSP and has an important reference value for clinical condition evaluations and treatment options.25 There was no investigation into the post-treatment changes in CSP features after MTX administration.
The small sample size and single-index observation were some of the limitations of this study. Further studies with a larger sample size are required to investigate the value of serial Doppler ultrasound examinations for follow-ups after the medical treatment of a CSP.
The results of this study demonstrated that serial Doppler ultrasound examination can be a useful method to evaluate the success or failure of medical management of CSPs, as the increase in RI values rapidly occurs after medical treatment and correlates well with blood β-hCG levels’ measurement.
Conclusion
The results of this study demonstrated that serial Doppler ultrasound examinations can be a useful method to evaluate the success or failure of medical management of CSPs as the increase in RI values occur rapidly after medical treatment and correlate well with blood β-hCG levels’ measurement.
Ethics statement
The current study with the code (IR.TBZMED.REC.1399.965) has been approved by the Ethics Committee of Tabriz University of Medical Sciences.
Conflict of interests declaration
The authors declare no conflict of interests.
Data availability statement
The datasets generated and analyzed during the current study are not publicly available due to individual privacy but are available from the corresponding author upon reasonable request.
Author contributions
Conceptualization: Elham Eghbali, Mahsa Karbasi.
Data curation: Mahsa Karbasi.
Formal analysis: Maryam Sodabi, Esmaeil Farhadi.
Investigation: Maryam Sodabi, Ali Nikoukhesal.
Methodology: Nima Ghanini, Esmaeil Farhadi.
Project administration: Elham Eghbali.
Resources: Alireza Omara Shahestan, Fatemeh Abbasalizadeh.
Software: Farzad Razmifard, Maryam Sodabi.
Supervision: Mahsa Karbasi, Elham Eghbali.
Validation: Farzad Razmifard, Nima Ghanini, Fatemeh Abbasalizadeh.
Visualization: Elham Eghbali, Mahsa Karbasi.
Writing–original draft: Maryam Sodabi, Nima Ghanini, Esmaeil Farhadi.
Writing–review & editing: Ali Nikoukhesal, Farzad Razmifard.
Consent for publication
Not applicable.
References
- Grechukhina O, Deshmukh U, Fan L, Kohari K, Abdel-Razeq S, Bahtiyar MO. Cesarean scar pregnancy, incidence, and recurrence: five-year experience at a single tertiary care referral center. Obstet Gynecol 2018; 132(5):1285-95. doi: 10.1097/aog.0000000000002940 [Crossref] [ Google Scholar]
- Riaz RM, Williams TR, Craig BM, Myers DT. Cesarean scar ectopic pregnancy: imaging features, current treatment options, and clinical outcomes. Abdom Imaging 2015; 40(7):2589-99. doi: 10.1007/s00261-015-0472-2 [Crossref] [ Google Scholar]
- Timor-Tritsch IE, Monteagudo A. Unforeseen consequences of the increasing rate of cesarean deliveries: early placenta accreta and cesarean scar pregnancy A review. Am J Obstet Gynecol 2012; 207(1):14-29. doi: 10.1016/j.ajog.2012.03.007 [Crossref] [ Google Scholar]
- Pędraszewski P, Wlaźlak E, Panek W, Surkont G. Cesarean scar pregnancy - a new challenge for obstetricians. J Ultrason 2018; 18(72):56-62. doi: 10.15557/JoU.2018.0009 [Crossref] [ Google Scholar]
- Gonzalez N, Tulandi T. Cesarean scar pregnancy: a systematic review. J Minim Invasive Gynecol 2017; 24(5):731-8. doi: 10.1016/j.jmig.2017.02.020 [Crossref] [ Google Scholar]
- Rheinboldt M, Osborn D, Delproposto Z. Cesarean section scar ectopic pregnancy: a clinical case series. J Ultrasound 2015; 18(2):191-5. doi: 10.1007/s40477-015-0162-5 [Crossref] [ Google Scholar]
- Liu H, Leng J, Shi H, Lang J. Expectant treatment of cesarean scar pregnancy: two case reports and a glimpse at the natural courses. Arch Gynecol Obstet 2010; 282(4):455-8. doi: 10.1007/s00404-010-1391-7 [Crossref] [ Google Scholar]
- Zhang Y, Gu Y, Wang JM, Li Y. Analysis of cases with cesarean scar pregnancy. J Obstet Gynaecol Res 2013; 39(1):195-202. doi: 10.1111/j.1447-0756.2012.01892.x [Crossref] [ Google Scholar]
- Knapman BL, Forgues MA, Abbott JA, Maheux-Lacroix S. Other treatments for CSP. Best Pract Res Clin Obstet Gynaecol 2023; 90:102367. doi: 10.1016/j.bpobgyn.2023.102367 [Crossref] [ Google Scholar]
- Chiang YC, Tu YA, Yang JH, Lin SY, Lee CN, Shih JC. Risk factors associated with failure of treatment for cesarean scar pregnancy. Int J Gynaecol Obstet 2017; 138(1):28-36. doi: 10.1002/ijgo.12157 [Crossref] [ Google Scholar]
- Tanaka K, Coghill E, Ballard E, Sekar R, Amoako A, Khalil A. Management of caesarean scar pregnancy with high dose intravenous methotrexate infusion therapy: 10-year experience at a single tertiary centre. Eur J Obstet Gynecol Reprod Biol 2019; 237:28-32. doi: 10.1016/j.ejogrb.2019.04.008 [Crossref] [ Google Scholar]
- Jayaram P, Okunoye G, Al Ibrahim AA, Ghani R, Kalache K. Expectant management of caesarean scar ectopic pregnancy: a systematic review. J Perinat Med 2018; 46(4):365-72. doi: 10.1515/jpm-2017-0189 [Crossref] [ Google Scholar]
- Shen L, Tan A, Zhu H, Guo C, Liu D, Huang W. Bilateral uterine artery chemoembolization with methotrexate for cesarean scar pregnancy. Am J Obstet Gynecol 2012;207(5):386.e1-386.e6. 10.1016/j.ajog.2012.09.012.
- Bartels HC, Brennan DJ, Timor-Tritsch IE, Agten AK. Global variation and outcomes of expectant management of CSP. Best Pract Res Clin Obstet Gynaecol 2023; 89:102353. doi: 10.1016/j.bpobgyn.2023.102353 [Crossref] [ Google Scholar]
- Zhou X, Li H, Fu X. Identifying possible risk factors for cesarean scar pregnancy based on a retrospective study of 291 cases. J Obstet Gynaecol Res 2020; 46(2):272-8. doi: 10.1111/jog.14163 [Crossref] [ Google Scholar]
- Jo EJ, Cha HH, Seong WJ. Delayed diagnosis of a cesarean scar pregnancy: a case report. J Med Case Rep 2019; 13(1):53. doi: 10.1186/s13256-019-1983-1 [Crossref] [ Google Scholar]
- Mo X, Tang S, Li C. Management for delayed diagnosis in cesarean scar pregnancy with hemorrhage intra- or postuterine dilation and curettage. J Obstet Gynaecol Res 2021; 47(6):2014-20. doi: 10.1111/jog.14771 [Crossref] [ Google Scholar]
- Timor-Tritsch IE, Monteagudo A, Calì G, D’Antonio F, Agten AK. Cesarean scar pregnancy: patient counseling and management. Obstet Gynecol Clin North Am 2019; 46(4):813-28. doi: 10.1016/j.ogc.2019.07.010 [Crossref] [ Google Scholar]
- Kim SY, Yoon SR, Kim MJ, Chung JH, Kim MY, Lee SW. Cesarean scar pregnancy; diagnosis and management between 2003 and 2015 in a single center. Taiwan J Obstet Gynecol 2018; 57(5):688-91. doi: 10.1016/j.tjog.2018.08.013 [Crossref] [ Google Scholar]
- Karahasanoglu A, Uzun I, Deregözü A, Ozdemir M. Successful treatment of cesarean scar pregnancy with suction curettage: our experiences in early pregnancy. Ochsner J 2018; 18(3):222-5. doi: 10.31486/toj.17.0118 [Crossref] [ Google Scholar]
- Ravi Selvaraj L, Rose N, Ramachandran M. Pitfalls in ultrasound diagnosis of cesarean scar pregnancy. J Obstet Gynaecol India 2018; 68(3):164-72. doi: 10.1007/s13224-016-0956-1 [Crossref] [ Google Scholar]
- Riaz RM, Williams TR, Craig BM, Myers DT. Cesarean scar ectopic pregnancy: imaging features, current treatment options, and clinical outcomes. Abdom Imaging 2015; 40(7):2589-99. doi: 10.1007/s00261-015-0472-2 [Crossref] [ Google Scholar]
- Huo X, Xie Y, Yang L, Deng K, Liu Y. Doppler ultrasound evaluation of the efficacy of high intensity focused ultrasound in treatment of cesarean section scar pregnancy. J Coll Physicians Surg Pak 2020; 30(3):240-4. doi: 10.29271/jcpsp.2020.03.240 [Crossref] [ Google Scholar]
- Timor-Tritsch IE, Monteagudo A, Santos R, Tsymbal T, Pineda G, Arslan AA. The diagnosis, treatment, and follow-up of cesarean scar pregnancy. Am J Obstet Gynecol 2012;207(1):44.e1-44.e13. 10.1016/j.ajog.2012.04.018.
- Shi L, Huang L, Liu L, Yang X, Yao D, Chen D. Diagnostic value of transvaginal three-dimensional ultrasound combined with color Doppler ultrasound for early cesarean scar pregnancy. Ann Palliat Med 2021; 10(10):10486-94. doi: 10.21037/apm-21-2208 [Crossref] [ Google Scholar]