Int J Drug Res Clin. 2:e6.
doi: 10.34172/ijdrc.2024.e6
Original Article
Effects of Oropharyngeal Lidocaine Spray Before Endotracheal Intubation on Heart Rate, Blood Pressure, and Arrhythmia in Patients Undergoing Coronary Artery Bypass Grafting Surgery: A Randomized Clinical Trial
Alireza Mahoori 1  , Reza Hajizadeh 2
, Reza Hajizadeh 2  , Sahar Ghodratizadeh 1, *
, Sahar Ghodratizadeh 1, *  , Behnam Askari 2
, Behnam Askari 2
Author information:
1Department of Anesthesiology, School of Medicine, Urmia University of Medical Sciences, Urmia, Iran
2Department of Cardiology, School of Medicine, Urmia University of Medical Sciences, Urmia, Iran
Abstract
Background:
Coronary artery disease is a growing disease in human societies. A considerable number of patients ultimately require coronary artery bypass graft (CABG) surgery. Laryngoscopy and endotracheal intubation in these patients may lead to increased heart rate (HR) and blood pressure (BP), which can exacerbate myocardial ischemia. This study aimed to investigate the potential effect of local lidocaine administration before endotracheal intubation on reducing atrial fibrillation attacks, BP changes, HR, length of hospital stay, and mortality in patients undergoing CABG surgery.
Methods:
In this randomized controlled clinical trial, a total of 60 candidates for CABG surgery were randomly divided into a lidocaine spray (LS) group with 30 patients and a control (C) group. Patients were randomly assigned to two groups by using computer software. In the LS group, two puffs of 10% LS were used before anesthesia induction and two puffs during laryngoscopy for endotracheal intubation. Distilled water spray was used in the C group. Mean arterial pressure (MAP) and HR at baseline (T0), one minute after anesthesia induction (T1), and in timeline durations after endotracheal intubation were measured and recorded. Finally, the patients were monitored for atrial fibrillation, length of stay in the intensive care unit (ICU), and in-hospital mortality.
Results:
The frequency of atrial fibrillation, length of hospital stay, and hospital mortality in patients receiving LS and the C group did not have a significant difference (P>0.05). The HR was significantly lower in patients in the LS group than in the C group two (T4), three (T5), five (T7), and ten (T8) minutes after intubation.
Conclusion:
This study showed that patients who received LS before intubation had better hemodynamic stability and a lower chance of tachycardia.
Keywords: Coronary artery bypass, Lidocaine, Arterial pressure, Heart rate, Arrhythmias, Cardiac
Copyright and License Information
© 2024 The Author(s).
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
None.
Please cite this article as follows: Mahoori A, Hajizadeh R, Ghodratizadeh S, Askari B. Effects of oropharyngeal lidocaine spray before endotracheal intubation on heart rate, blood pressure, and arrhythmia in patients undergoing coronary artery bypass grafting surgery: a randomized clinical trial. Int J Drug Res Clin. 2024; 2: e6. doi: 10.34172/ijdrc.2024.e6
Introduction
Coronary artery disease is an important concern in human societies, reducing the life expectancy of individuals and imposing a substantial cost on healthcare systems. In some countries, ischemic heart disease has higher mortality and morbidity than cancer and road accidents. Although interventions such as angiography and the use of cardiac stents to open occluded arteries are feasible for many patients, some patients finally require coronary artery bypass graft (CABG) surgery. Arrhythmias and conduction disturbances are commonly observed after this surgery, leading to prolonged hospitalization and an increased risk of stroke.1
During the induction of anesthesia for CABG, direct laryngoscopy and endotracheal intubation are significant stimuli that can result in unwanted responses in the cardiovascular, respiratory, and other physiological systems. While hemodynamic changes begin with premedication and the induction of anesthesia, the major changes, such as increased heart rate (HR), arrhythmias, and blood pressure (BP), are observed moments after direct laryngoscopy and endotracheal intubation. These changes peak 1–2 minutes after laryngoscopy and usually return to baseline levels within 5 minutes. These transient changes are well tolerated by healthy individuals, but in susceptible patients, especially those with systemic hypertension, coronary artery disease, abdominal aortic aneurysm, intracranial aneurysm, recent myocardial infarction, and those undergoing coronary artery bypass surgery, sudden changes in HR and BP can cause serious problems.2
In the respiratory system and airways, bronchospasm and bronchiolar spasm can pose additive risks. These stimuli can occasionally lead to arrhythmias such as atrial fibrillation, which is one of the most common arrhythmias after coronary artery bypass surgery.3 While these arrhythmias are self-limiting, they increase the length of hospital stays, leading to increased costs.4
A recent study has shown that the duration of intubation in the intensive care unit (ICU) is the strongest predictor of 30-day and one-year mortality in patients with heart failure undergoing CABG. Various pharmacologist techniques have been utilized to reduce unwanted hemodynamic responses, such as deepening anesthesia, vasodilators, calcium channel blockers, and opioids, with variable results.5
One study by Bilgi et al demonstrated that the use of 10% lidocaine spray (LS) 5 minutes before intubation in CABG surgery significantly affected QT dispersion duration, a potential factor in increasing the risk of cardiac arrhythmias.6 Another study suggested that intubation is associated with changes in stress-related parameters.7
There are few studies investigating the effect of routine use of topical lidocaine before intubation in CABG patients and the patient outcomes post-surgery. Finding a safe and cost-effective method to reduce post-surgical complications is important, and this study sought to examine the potential impact of topical lidocaine on hemodynamic stability and outcomes in CABG patients.
Methods
This double-blinded randomized control trial was designed to investigate the effects of LS in patients undergoing CABG surgery. In this trial, 60 patients were divided into LS and control groups, and consent for the anesthesia method was obtained from all patients. Patients with specific conditions such as previous arrhythmias, cardiomyopathy, renal and hepatic dysfunction, lidocaine sensitivity, and specific respiratory problems were excluded from the investigation. Twenty-five patients were randomly assigned to two groups by using computer software, which was utilized for random allocation. In the lidocaine group, 2 puffs of 10% LS (Iran Darou©) were used before inducing anesthesia and tracheal intubation, while in the control group, distilled water spray was used. This trial was performed in one tertiary center, which is the main referral hospital for surgery cases located in the northwest of Iran.
Similar containers with labels A and B were used to ensure that the physicians were unaware of the type of applied spray. Only the clinical pharmacology responsible in the hospital was aware of the content of each spray, and to reduce the bias of the smell of LS, the attending physician who intubated the patient using LS and the physician who recorded the patient’s symptoms were different.
The treating physician and the researcher responsible for analyzing and monitoring data were unaware of the type of spray used, making this a double-blind study. The anesthesia method was the same for all patients. Following pre-medication with midazolam and fentanyl, an arterial line for BP monitoring was established using a 20-gauge angiocath. Baseline vital signs, including mean arterial pressure (MAP) using central pressure monitoring, HR, and arterial oxygen saturation, were assessed and recorded.
In the LS group, lidocaine was sprayed into the back of the tongue and around the glottis before inducing anesthesia, and after consistent induction of anesthesia with midazolam, fentanyl, and cisatracurium, LS was administered again to the vocal cords and trachea following laryngoscopy. Subsequently, endotracheal intubation was performed using size 8.5 and 7.5 tubes for males and females, respectively. Anesthesia maintenance for all patients was achieved using isoflurane in oxygen, and propofol infusion was used during cardiopulmonary bypass. Patients taking vasoactive drugs were excluded from the study.
MAP, HR, and arterial oxygen saturation were measured and recorded at baseline (T0), one minute after induction of anesthesia (T1), 30 seconds (T2), and one (T3), two (T4), three (T5), four (T6), five (T7), and 10 (T8) minutes after endotracheal intubation. During ICU and hospital stays, the patients were followed for atrial fibrillation, length of stay in the ICU, and hospital mortality.
Data on patient characteristics were presented using descriptive statistics (means and standard deviations). Data analysis involved the use of the chi-square test (or Fisher’s exact test as needed) for comparing frequencies between the two groups, the independent t-test for comparing means, and repeated measurements analysis (Friedman test if necessary) for comparing quantitative outcomes over time intervals. Statistical analysis was performed using SPSS, version 17.
According to the study by Bilgi et al,6 at least 30 people were determined in each group, considering the 95% confidence interval (Z1-α/2 = 1.96) and the power of the test at 80% (Z1-β = 0.84).
Results
In this study, patients undergoing coronary artery bypass surgery were examined and divided into two LS (n = 30) and control (n = 30) groups. The average weight of the patients in the lidocaine and control groups was 72.7 ± 3.61 kg and 71.9 ± 59 kg, respectively. In the LS group, 63.3% were male, and in the control group, 56.7% were male. Figure 1 shows the consort chart for patient selection.
Figure 1.
Consort Chart for Patient Selection
.
Consort Chart for Patient Selection
Based on our findings, the frequency of atrial fibrillation in patients receiving LS and the control group after surgery during recovery demonstrated no significant difference (P > 0.05, Figure 2).
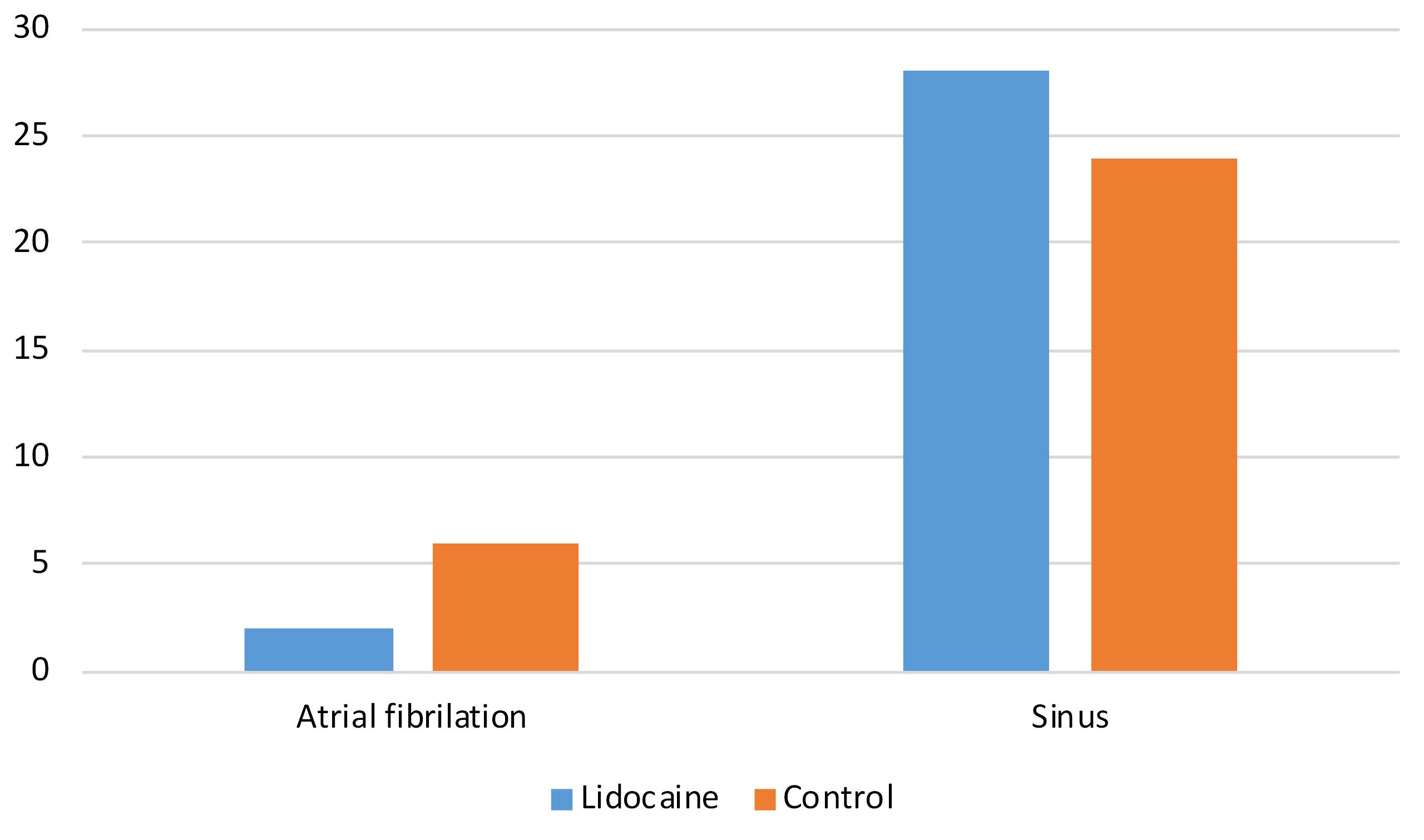
Figure 2.
The Frequency of Atrial Fibrillation in Patients in the Lidocaine Spray Recipient Group and the Control Group During the Recovery After Surgery
.
The Frequency of Atrial Fibrillation in Patients in the Lidocaine Spray Recipient Group and the Control Group During the Recovery After Surgery
Table 1 compares the mean HR at baseline (T0), one minute after anesthesia induction (T1), 30 seconds (T2), one minute (T3), and four (T6) after intubation in patients in the two groups. The independent samples t-test revealed that there was no significant difference in the HR at baseline (T0), one minute after anesthesia induction (T1), 30 seconds (T2), one minute (T3), and four (T6) after intubation in the two groups (P > 0.05). However, a significant difference was observed in the HR at two (T4), three (T5), five (T7), and ten (T8) minutes after intubation in patients in the two groups receiving LS and the control group (P < 0.05). The mean HR was lower in the LS group.
Table 1.
The Average Heart Rate at Different Time Points in Patients in Both the Lidocaine Spray and Control Groups
|
|
Lidocaine Group
|
Control Group
|
T-test Value
|
P
Value
|
| HR.T0 |
77.0 ± 16.9 |
82.5 ± 10.5 |
-1.503 |
0.138 |
| HR.T1 |
71.4 ± 19.2 |
74.0 ± 9.9 |
-0.659 |
0.513 |
| HR.T2 |
69.1 ± 13.5 |
74.6 ± 11.3 |
-1.699 |
0.095 |
| HR.T3 |
69.6 ± 15.3 |
75.0 ± 9.3 |
-1.656 |
0.103 |
| HR.T4 |
65.0 ± 13.5 |
74.7 ± 9.1 |
-3.264 |
0.002 |
| HR.T5 |
64.3 ± 14.6 |
71.9 ± 8.5 |
-2.472 |
0.016 |
| HR.T6 |
66.0 ± 15.9 |
71.4 ± 9.2 |
-1.601 |
0.115 |
| HR.T7 |
65.7 ± 16.4 |
72.7 ± 8.5 |
-2.067 |
0.042 |
| HR.T8 |
65.2 ± 15.0 |
71.8 ± 7.4 |
-2.156 |
0.035 |
Based on the results of Table 2, the MAP was not significantly different in the two groups at baseline (T0), one minute after anesthesia induction (T1), 30 seconds (T2), one minute (T3), three (T5), four (T6), five (T7), and ten (T8) minutes after intubation, and only the MAP was significantly lower in the LS group after two minutes of intubation.
Table 2.
Comparison of the Mean Arterial Pressure at Different Time Points in Patients in the Lidocaine Spray and Control Groups
|
|
Lidocaine Group
|
Control Group
|
T-test Value
|
P
Value
|
| MAP.T0 |
109.3 ± 29.8 |
97.4 ± 9.8 |
2.075 |
0.138 |
| MAP.T1 |
89.7 ± 12.1 |
88.6 ± 7.9 |
0.441 |
0.661 |
| MAP.T2 |
79.4 ± 12.4 |
83.1 ± 8.6 |
-1.311 |
0.195 |
| MAP.T3 |
77.0 ± 12.3 |
80.1 ± 8.0 |
-1.172 |
0.246 |
| MAP.T4 |
74.5 ± 8.1 |
79.1 ± 6.1 |
-2.469 |
0.016 |
| MAP.T5 |
76.1 ± 10.2 |
78.1 ± 6.6 |
-0.901 |
0.371 |
| MAP.T6 |
76.3 ± 8.8 |
78.6 ± 7.2 |
-1.139 |
0.261 |
| MAP.T7 |
77.2 ± 10.7 |
77.8 ± 7.3 |
-0.23 |
0.812 |
| MAP.T8 |
77.6 ± 9.1 |
77.5 ± 7.2 |
0.063 |
0.950 |
The length of ICU stay was 0.6 ± 2.2 and 0.3 ± 2.1 days in the LS and control groups, respectively (P = 0.474). There was no significant difference in in-hospital mortality between the patients in the LS and control groups (P = 0.313).
The mean percentage of oxygen saturation was measured by pulse oximetry (SpO2) in the two groups. Although SpO2 was lower in the LS group at the base time, patients in the lidocaine group had significantly higher SpO2 after intubation.
No significant difference was found between the two groups regarding in-hospital mortality or the length of the recovery room observation.
Discussion
Lidocaine as a medium-acting agent is used to relieve pain, and its short onset of action makes it the drug of choice in many emergency conditions.8 Previous studies have failed to find drugs that could improve hemodynamic stability during rapid intubation.9 This study aimed to investigate the effect of oropharyngeal LS before tracheal intubation on HR, BP, and arrhythmia in patients undergoing heart surgery. Laryngoscopy and intubation are stressful as they lead to an increase in HR and BP.10 The hemodynamic response to laryngoscopy and intubation, which is characterized by tachycardia and increased BP, is well known. It is believed that the stimulation of mechanoreceptors in the tracheal wall, epiglottis, and vocal cords is the cause of this hemodynamic response.
Elevated HR is recognized as an independent predictor of adverse events after surgery. Previous studies have shown that for every 20 beats per minute increase in HR, the chance of intraoperative mortality increases by 3050%.11 A higher HR during surgery is considered a risk factor for postoperative myocardial infarction.12 Preventing an increase in HR using beta-blockers is of particular importance in non-cardiac surgeries, especially in vascular surgeries.13,14
Reich et al demonstrated that an HR > 100 beats per minute in the early postoperative period is an independent risk factor for postoperative myocardial infarction, but it has no impact on stroke or postoperative mortality.15
Furthermore, Fillinger et al reported that an HR of over 80 beats per minute before the induction of anesthesia is associated with increased mortality. All these studies used human resources recorded during a very close period to CABG surgery in operating room.16 Shribman et al concluded that laryngoscopy alone or following intubation increases arterial pressure and catecholamine levels, and intratracheal tube insertion is significantly associated with an increase in HR.17 These changes reach their maximum rate 60 seconds after intratracheal tube insertion and take 5–10 minutes to resolve. If no specific measures are taken to prevent this hemodynamic response, the patient’s HR can increase by 26%–66%, and systolic BP can increase by 36%–45%. These effects are more harmful in patients with high BP.17,18
The findings of the present study revealed that there was no significant difference in the frequency of atrial fibrillation between patients receiving LS and the control group during heart surgery recovery (P> 0.05).
The force applied by the laryngoscope at the base of the tongue during the lifting of the epiglottis is responsible for the hemodynamic response to laryngoscopy and intubation.19
In our study, LS had a greater effect on HR than arterial pressure. It seems that after laryngoscopy and endotracheal tube insertion, a stable period without sudden increases or decreases in arterial pressure was achieved using local lidocaine. However, this decrease in HR and BP at certain time intervals can also be attributed to the combined effects of fentanyl and inhalation agents administered during anesthesia maintenance.
In line with our findings, Lee et al demonstrated that the MAP at 5 and 2.5 minutes and HR at 5 minutes were significantly higher in the control group than in the 10% LS group. They used LS on the laryngeal and intratracheal tissues of patients 2 minutes before intubation.20
As observed in the study by Shribman et al, the primary cause of the sympathetic adrenal response after laryngoscopy and endotracheal tube insertion is the supraglottic pressure with the laryngoscope blade and the stimulation of the mucosa with the endotracheal tube. Topical lidocaine administration may reduce this stimulation and consequently prevent sympathetic adrenergic secretion.17,21
Mostafa et al found that LS before anesthesia induction is an effective method for controlling the pressor response in patients undergoing laryngoscopy or intubation.7 Although this study with a limited sample size could not give exact recommendations about the administration of LS for all patients, the results of this study could help physicians in some patients when routine interventions fail to maintain hemodynamic stability, especially in those patients who had hemodynamic instability in previous tracheal intubations and needed re-intubation. Golzari et al reported that lidocaine is used safely in many patients with different diseases through various roots.22
Limitations of the Study
The main limitation of our study was the relatively small number of patients. Conducting the study on a larger population can increase the statistical power of our study. However, we did not match the left ventricular ejection fraction in the two groups, which could affect hemodynamic changes. In addition, some patients used beta-blockers before the operation. Although randomization could match the two groups to some degree, drugs used before surgery could affect our results.
Conclusion
Our findings confirmed that patients who received LS before intubation had better hemodynamic stability and a lower chance of tachycardia.
Ethics statement
The study was initiated after obtaining approval from the university’s ethics committee with an IRCT ID of IRCT20170411033365N3 in 2022.3.15. Informed consent for participation in the study was obtained from all patients, and patient confidentiality was maintained. The datasets used during the current study are available from the corresponding author upon reasonable request.
Conflict of interests declaration
The authors declare no conflict of interests.
Data availability statement
The data that support the findings of this study are available on request from the corresponding author Email address.
Author contributions
Conceptualization: Alireza Mahoori.
Data curation: Sahar Ghodratizadeh.
Formal analysis: Reza Hajizadeh.
Investigation: Behnam Askari.
Methodology: Alireza Mahoori.
Project administration: Alireza Mahoori.
Resources: Sahar Ghodratizadeh.
Supervision: Alireza Mahoori.
Validation: Behnam Askari.
Visualization: Sahar Ghodratizadeh.
Writing–original draft: Reza Hajizadeh.
Writing–review & editing: Reza Hajizadeh.
Consent for publication
Written informed consent was obtained from all patients. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Iribarne A, DiScipio AW, Leavitt BJ, Baribeau YR, McCullough JN, Weldner PW, et al. Comparative effectiveness of coronary artery bypass grafting versus percutaneous coronary intervention in a real-world surgical treatment for ischemic heart failure trial population. J Thorac Cardiovasc Surg 2018;156(4):1410-21.e2. 10.1016/j.jtcvs.2018.04.121.
- Parida S, Ashraf NC, Mathew JS, Mishra SK, Badhe AS. Attenuation of the haemodynamic responses to tracheal intubation with gabapentin, fentanyl and a combination of both: a randomised controlled trial. Indian J Anaesth 2015; 59(5):306-11. doi: 10.4103/0019-5049.156885 [Crossref] [ Google Scholar]
- Zaman AG, Archbold RA, Helft G, Paul EA, Curzen NP, Mills PG. Atrial fibrillation after coronary artery bypass surgery: a model for preoperative risk stratification. Circulation 2000; 101(12):1403-8. doi: 10.1161/01.cir.101.12.1403 [Crossref] [ Google Scholar]
- Ismail MF, El-Mahrouk AF, Hamouda TH, Radwan H, Haneef A, Jamjoom AA. Factors influencing postoperative atrial fibrillation in patients undergoing on-pump coronary artery bypass grafting, single center experience. J Cardiothorac Surg 2017; 12(1):40. doi: 10.1186/s13019-017-0609-1 [Crossref] [ Google Scholar]
- Bouabdallaoui N, Stevens SR, Doenst T, Wrobel K, Bouchard D, Deja MA. Impact of intubation time on survival following coronary artery bypass grafting: insights from the surgical treatment for ischemic heart failure (STICH) trial. J Cardiothorac Vasc Anesth 2018; 32(3):1256-63. doi: 10.1053/j.jvca.2017.12.038 [Crossref] [ Google Scholar]
- Bilgi M, Velioglu Y, Yoldas H, Cosgun M, Yuksel A, Karagoz I. Effects of lidocaine oropharyngeal spray applied before endotracheal intubation on QT dispersion in patients undergoing coronary artery bypass grafting: a prospective randomized controlled study. Braz J Cardiovasc Surg 2020; 35(3):291-8. doi: 10.21470/1678-9741-2019-0112 [Crossref] [ Google Scholar]
- Mostafa SM, Murthy BV, Barrett PJ, McHugh P. Comparison of the effects of topical lignocaine spray applied before or after induction of anaesthesia on the pressor response to direct laryngoscopy and intubation. Eur J Anaesthesiol 1999; 16(1):7-10. doi: 10.1046/j.1365-2346.1999.00410.x [Crossref] [ Google Scholar]
- Ghojazadeh M, Sanaie S, Parsian Z, Najafizadeh R, Soleimanpour H. Use of lidocaine for pain management in the emergency medicine: a systematic review and meta-analysis. Pharm Sci 2019; 25(3):177-83. doi: 10.15171/ps.2019.48 [Crossref] [ Google Scholar]
- Pouraghaei M, Moharamzadeh P, Soleimanpour H, Rahmani F, Safari S, Mahmoodpoor A. Comparison between the effects of alfentanil, fentanyl and sufentanil on hemodynamic indices during rapid sequence intubation in the emergency department. Anesth Pain Med 2014; 4(1):e14618. doi: 10.5812/aapm.14618 [Crossref] [ Google Scholar]
- Lakhe G, Pradhan S, Dhakal S. Hemodynamic response to laryngoscopy and intubation using McCoy laryngoscope: a descriptive cross-sectional study. JNMA J Nepal Med Assoc 2021; 59(238):554-7. doi: 10.31729/jnma.6752 [Crossref] [ Google Scholar]
- Aboyans V, Frank M, Nubret K, Lacroix P, Laskar M. Heart rate and pulse pressure at rest are major prognostic markers of early postoperative complications after coronary bypass surgery. Eur J Cardiothorac Surg 2008; 33(6):971-6. doi: 10.1016/j.ejcts.2008.01.065 [Crossref] [ Google Scholar]
- Slogoff S, Keats AS. Does perioperative myocardial ischemia lead to postoperative myocardial infarction?. Anesthesiology 1985; 62(2):107-14. doi: 10.1097/00000542-198502000-00002 [Crossref] [ Google Scholar]
- Mangano DT, Layug EL, Wallace A, Tateo I. Effect of atenolol on mortality and cardiovascular morbidity after noncardiac surgery Multicenter Study of Perioperative Ischemia Research Group. N Engl J Med 1996; 335(23):1713-20. doi: 10.1056/nejm199612053352301 [Crossref] [ Google Scholar]
- Schonberger RB, Brandt C, Feinleib J, Dai F, Burg MM. Atenolol is associated with lower day-of-surgery heart rate compared to long- and short-acting metoprolol. J Cardiothorac Vasc Anesth 2013; 27(2):298-304. doi: 10.1053/j.jvca.2012.06.021 [Crossref] [ Google Scholar]
- Reich DL, Bodian CA, Krol M, Kuroda M, Osinski T, Thys DM. Intraoperative hemodynamic predictors of mortality, stroke, and myocardial infarction after coronary artery bypass surgery. Anesth Analg 1999; 89(4):814-22. doi: 10.1097/00000539-199910000-00002 [Crossref] [ Google Scholar]
- Fillinger MP, Surgenor SD, Hartman GS, Clark C, Dodds TM, Rassias AJ. The association between heart rate and in-hospital mortality after coronary artery bypass graft surgery. Anesth Analg 2002; 95(6):1483-8. doi: 10.1097/00000539-200212000-00005 [Crossref] [ Google Scholar]
- Shribman AJ, Smith G, Achola KJ. Cardiovascular and catecholamine responses to laryngoscopy with and without tracheal intubation. Br J Anaesth 1987; 59(3):295-9. doi: 10.1093/bja/59.3.295 [Crossref] [ Google Scholar]
- Dashti M, Amini S, Azarfarin R, Totonchi Z, Hatami M. Hemodynamic changes following endotracheal intubation with GlideScope® video-laryngoscope in patients with untreated hypertension. Res Cardiovasc Med 2014; 3(2):e17598. doi: 10.5812/cardiovascmed.17598 [Crossref] [ Google Scholar]
- Safavi M, Honarmand A. Attenuation of cardiovascular responses to laryngoscopy and tracheal intubation--intravenous sufentanil vs pethidine. Middle East J Anaesthesiol 2008; 19(6):1349-59. [ Google Scholar]
- Lee DH, Park SJ. Effects of 10% lidocaine spray on arterial pressure increase due to suspension laryngoscopy and cough during extubation. Korean J Anesthesiol 2011; 60(6):422-7. doi: 10.4097/kjae.2011.60.6.422 [Crossref] [ Google Scholar]
- Kaneko M, Yamaguchi S, Hamaguchi S, Egawa H, Fujii K, Ishikawa K. Effects of landiolol on QT interval and QT dispersion during induction of anesthesia using computerized measurement. J Clin Anesth 2009; 21(8):555-61. doi: 10.1016/j.jclinane.2008.12.027 [Crossref] [ Google Scholar]
- Golzari S, Soleimanpour H, Mahmoodpoor A, Safari S, Ala A. Lidocaine and pain management in the emergency department: a review article. Anesth Pain Med 2014; 4(1):e15444. doi: 10.5812/aapm.15444 [Crossref] [ Google Scholar]