Int J Drug Res Clin. 2023;1:e5.
doi: 10.34172/ijdrc.2023.e5
Original Article
The Effects of Urtica dioica (Nettle) and Vaccinium myrtillus (European Blueberry) on Blood Glucose Parameters and Lipid Profile in Patients With Type 2 Diabetes Mellitus: A Double-Blind Randomized Controlled Trial
Anita Chehri 1  , Reza Yarani 2, Zahra Yousefi 3, Seyed Kazem Shakouri 4, Alireza Ostadrahimi 5, Majid Mobasseri 5, Reza Majidazar 6, Mostafa Araj-khodaei 7, *
, Reza Yarani 2, Zahra Yousefi 3, Seyed Kazem Shakouri 4, Alireza Ostadrahimi 5, Majid Mobasseri 5, Reza Majidazar 6, Mostafa Araj-khodaei 7, * 
Author information:
1Department of Persian Medicine, Faculty of Traditional Medicine, Tabriz University of Medical Sciences, Tabriz, Iran
2Translational Type 1 Diabetes Research, Department of Clinical Research, Steno Diabetes Center Copenhagen, Gentofte, Denmark
3Psychiatry Research Center, Aging Research Institute, Tabriz University of Medical Sciences, Tabriz, Iran
4Physical Medicine Research Center, Aging Research Institute, Tabriz University of Medical Sciences, Tabriz, Iran
5Department of Clinical Nutrition, School of Nutrition and Food Sciences, Tabriz University of Medical Sciences, Tabriz, Iran
6Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran
7Aging Research Institute, Tabriz University of Medical Sciences, Tabriz, Iran
Abstract
Background:
Diabetes mellitus (DM), and more specifically type 2 DM (T2DM), is a growing metabolic disease and is accompanied by changes in lipid profile and glycemic parameters which contribute to debilitating complications. Nettle and European blueberry as complementary herbal medicine could play a significant role in managing elevated levels of blood sugar and diabetic complications. The goal of this study was to determine the effects of nettle and European blueberry combination as adjunct therapy in patients with T2DM.
Methods:
The randomized double-blind clinical trial included 59 T2D patients with a mean age of 57.9 years. Participants were randomly assigned to two groups to take either nettle-bilberry capsules (500/mg/dose twice a day, n=29) or a placebo (n=30) for three months. Fasting blood samples were obtained at the beginning and after the intervention to quantify 15 items, including lipid profile and glycemic factors.
Results:
Sixty patients were enrolled in this study. The groups had no significant difference regarding the demographics and the study variables at the baseline. Compared with the placebo, the nettle-bilberry combination resulted in significant decreases in fasting blood sugar (FBS), triglyceride, cholesterol, and low-density lipoprotein (LDL) levels (P<0.001). There was no statistically significant difference in the other indices, including glycated hemoglobin (HbA1c), urea, creatinine, high-density lipoproteins, liver function tests (LFTs), C-reactive protein (CRP), insulin, and insulin resistance (HOMAIR) levels (P>0.05).
Conclusion:
Overall, a combination of nettle and bilberry had beneficial impacts on the levels of FBS, cholesterol, and LDL. However, this combination had no significant effects on the other glycemic factors and lipid profile indicators.
Trial Registration:
This study was a double-blind randomized controlled trial study that was registered in the Iranian Registry of Clinical Trials (IRCT: IRCT20140617018126N3). In addition, approval was obtained from the Ethics Committee of Tabriz University of Medical Sciences (Ethics code: IR.TBZMED.REC.1399.093).
Keywords: Diabetes mellitus, Urtica dioica, Vaccinium myrtillus, Randomized Controlled Trial, Traditional medicine
Introduction
Diabetes mellitus (DM) is a metabolic disease in which the blood sugar of a person is higher than normal.1 DM is categorized into two distinct groups, namely, type 1 (T1DM) and type 2 (T2DM). In T1DM, which is insulin-dependent and is called juvenile/premature diabetes, the AIN dysfunction is in the production of insulin. T2DM, which was formerly known as adulthood or insulin-independent diabetes, is a chronic disease related to a lack of balance in glucose metabolism.1,2,3 The most recent global evaluation on the burden of different diseases on societies estimated that over half a billion people all over the world had T2DM, and 22 million new cases will be added every year.4,5 It is estimated that the number of people with T2DM will increase to 693 million by 2045.5 According to estimates by the World Health Organization in 2016, the prevalence of DM in Iran stands at 10.3%, and almost 2% of mortalities are directly caused by DM.6 Several risk factors play a role in T2DM, and the most important of them are race, family history, old age, higher body weight or obesity, unhealthy diet, lack of mobility or activity, high blood pressure, and smoking.1,3,7
Nettle is a medicinal plant with the scientific name Urtica dioica, which belongs to the Urticaceae family.8 This plant is found in the rural areas of North America, northern Europe, and various locations in Asia.7 It is widely used in Turkey and Morocco to control blood sugar.9 This plant is rich in formic acid and flavonoids.10 Numerous studies have shown the effect of nettle on different conditions, including rheumatoid arthritis, DM, urinary tract infections, prostate enlargement, seasonal allergies, and acne.11,12 An eight-week, double-blind, randomized controlled clinical trial (RCT) demonstrated that the hydro-alcoholic extract of U. dioica is an effective additional therapy for DM.13
Vaccinium myrtillus or European blueberry or bilberry is native to Europe and is one of the richest natural sources of anthocyanins. Bilberry is a source of dietary anthocyanin, which is a crucial dietary factor associated with DM.14 Several studies reported reducing blood glucose, anti-inflammatory, and lipid reduction properties for berries.15 It also strengthens antioxidant defense and lowers oxidative stress.16
Due to the reported efficacy of these herbal components and the lack of reliable evidence, this study aimed to investigate the effects of the combination of U. dioica and V. myrtillus on blood glucose parameters, lipid profile, kidney and liver function, and inflammation in patients with T2DM.
Methods
This was a double-blind RCT study. An eligible sample was selected after registering the study in the Iranian Registry of Clinical Trials (identifier: IRCT20140617018126N3) and obtaining approval from the Ethics Committee of Tabriz University of Medical Sciences (Ethics code: IR.TBZMED.REC.1399.093).
Inclusion Criteria
-
T2DM
-
Regular oral use of hypoglycemic agents (people who only take glucose-lowering drugs to control DM)
-
Age 40-70
-
Body mass index (BMI) of 18.5-30 kg/m2
-
Fasting blood sugar (FBS) level higher than 126 mg/dL
-
Willingness to take part in the present study.
Exclusion Criteria
-
T1DM or the other types of diabetes
-
Episodes of insulin therapy in the past three months
-
Serious gastrointestinal (GI) diseases, including peptic ulcer and GI bleeding
-
History of diabetic ketoacidosis, non-ketotic hyperosmolar diabetic coma, severe infection, or surgery in the previous month
-
Uncontrolled hypertension (blood pressures equal to or above 160/100 mm Hg)
-
History of mental illnesses
-
History of alcohol, drug, or psychedelic abuse
-
Pregnancy, lactation, or planning to become pregnant
-
Cardiovascular diseases, kidney failure, liver dysfunction, thyroid or parathyroid dysfunctions, and cancers
-
High physical activities
-
Chronic complications related to DM (e.g., neuropathy or retinopathy according to the patient’s records), diabetic nephropathy, hypothyroidism, and hyperthyroidism
-
Allergy to Nettle and V. myrtillus or their derivatives.
Patient’s Selection
The researcher in charge of selecting the population received a list of T2DM patients from the East Azerbaijan Diabetes Association and randomly selected participants for the present study using a table of random numbers. Then, this researcher contacted the selected participants and briefed them about the study and its aims while matching selected peoples’ conditions with the inclusion and exclusion criteria. In case the selected participants met the eligibility criteria and were willing to participate in the study, they could participate in this study.
Randomization and Random Allocation
The samples were randomly assigned to four blocks using Random Allocation Software. Blocking and allocation sequences for concealment were performed by the non-involved researcher. The sample allocation ratio was Allocation 1:1 and was divided into two groups of receiving U. dioica and V. myrtillus (nettle-bilberry/active intervention group), and placebo. Then, based on blocks and allocation sequences, each patient was given white pockets that were prepared in equal sizes and on which numbers 1 to 60 were written in order of the allocation sequence. The pockets included white boxes containing nettle-bilberry or placebo capsules. Only the person in charge of packing the capsules knew the numbers of the relevant pockets, and none of the researchers or patients were aware of the type of medicine that each person receives.
Plant Preparation
Nettle-bilberry and placebo capsules were similar in shape, size, color, and smell. Both identical nettle-bilberry and placebo capsules placed inside the white boxes were to be taken along with food by the participants every 12 hours (BID) for three months. Each 500 mg nettle-bilberry capsule contained 300 mg of nettle and 150 mg of bilberry along with filler material. Each placebo capsule consisted of 500 mg of a placebo. The participants were advised to continue taking their regularly prescribed medicines. The raw materials of herbs were collected from the rural areas of East Azerbaijan.
Data Collection
This study was conducted between March and September of 2021, and patients had been taking medications for three months. To collect personal information of the participant, a questionnaire was handed out, which contained demographic information, including age, gender, level of education, a brief history of medicines and supplements presently used and their doses and the duration, history of special diets (if any), current illnesses and disorders, and history of diabetes. Fasting blood samples of the participant were taken, and their weight, height, BMI, waist size, wrist size along with urine samples and blood pressure were recorded after having breakfast. The medication intake questionnaire was used to obtain data about medications taken by the participants.
Sample Size
The sample size for the present study was calculated based on previous studies and by considering the results obtained from G*Power software (Power: 0.095, significance level (α): 0.05, and SD: 28.5 to be 27 people for each group). By taking into account a 15% dropout, the final sample size was taken to be 30 people in each group and a total of sixty people.
Statistics
All statistical analyses were conducted using the 23rd version of SPSS software with 95% confidence intervals (CIs) and a 0.05 level of significance for the P value. The quantitative variables were reported as means ± standard deviations (SDs), and the qualitative data were presented in numbers and percentages. Finally, independent sample t test, chi-square test, and Mann-Whitney U test were employed for comparing the variables between the groups.
Results
Sixty patients (30 per group) were enrolled in this study. During the trial, one of the intervention group participants left the study because of personal reasons, and the final count of the participants in the intervention group was 29 (Figure 1). The obtained results demonstrated that the two understudy groups had no significant difference in terms of demographics and the study variables at the baseline (Table 1).
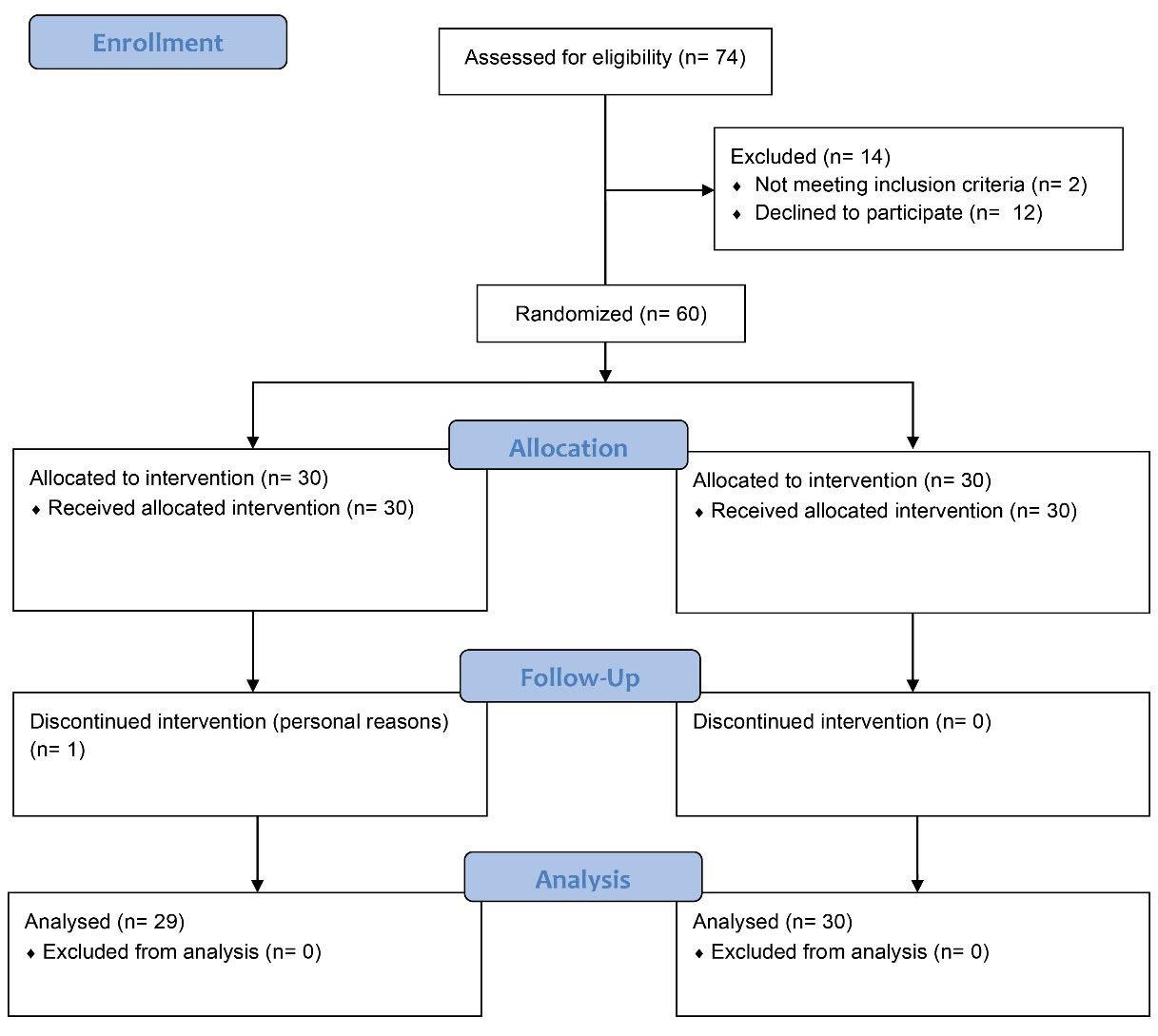
Figure 1.
CONSORT Flow Diagram.
.
CONSORT Flow Diagram.
Table 1.
Baseline Characteristics of Participants in the Study Groups
|
Variable
|
Intervention (n=29)
|
Placebo (n=30)
|
P
Value
|
| Age (year) |
57.17 ± 4.10 |
58.70 ± 4.17 |
0.161* |
| Gender |
Male |
17 (56.67%) |
14 (48.28%) |
0.519** |
| Female |
13 (43.33%) |
15 (51.72%) |
| Used medication |
Metformin |
18 (60.00%) |
10 (34.48%) |
0.927*** |
| Glibenclamide |
0 (0.00%) |
0 (0.00%) |
| Metformin and Glibenclamide |
10 (33.33%) |
10 (34.48%) |
| None |
2 (6.67%) |
3 (10.34%) |
| Other underlying diseases |
Positive |
5 (16.67%) |
6 (20.69%) |
0.692 |
| Negative |
25 (83.33%) |
23 (79.31%) |
| BMI |
27.44 ± 3.67 |
28.09 ± 1.93 |
0.392* |
| FBS |
129.41 ± 37.58 |
142.50 ± 39.31 |
0.197* |
| HbA1C |
7.6 ± 0.62 |
7.14 ± 39.31 |
0.327* |
| Urea |
31.55 ± 4.13 |
32.1031.55 ± 4.134.78 |
0.640* |
| BUN |
14.79 ± 2.01 |
14.73 ± 2.26 |
0.915* |
| Creatinine |
0.72 ± 0.11 |
0.76 ± 0.13 |
0.236* |
| Triglyceride |
114.63 ± 46.24 |
117.33 ± 29.68 |
0.789* |
| Cholesterol |
154.90 ± 37.73 |
160.27 ± 37.93 |
0.588* |
| HDL |
44.00 ± 4.93 |
42.33 ± 4.44 |
0.177* |
| LDL |
94.93 ± 29.41 |
103.27 ± 22.14 |
0.223* |
| AST |
20.86 ± 6.46 |
18.0 ± 6.74 |
0.102* |
| ALT |
19.31 ± 7.19 |
21.37 ± 6.93 |
0.268* |
| ALP |
147.21 ± 18.79 |
154.97 ± 19.97 |
0.130* |
| CRP |
2.82 ± 1.08 |
2.37 ± 0.95 |
0.095* |
| Insulin |
13.72 ± 5.47 |
14.52 ± 7.32 |
0.640* |
| Insulin resistance (HOMAIR) |
2.73 ± 0.27 |
2.82 ± 0.22 |
0.149* |
Note. BMI: Body mass index; FBS: Fasting blood sugar; HbA1C: Hemoglobin A1C; BUN: Blood urea nitrogen; HDL: High-density lipoprotein; LDL: Low-density lipoprotein; AST: Aspartate aminotransferase; ALT: Alanine aminotransferase; ALP: Alkaline phosphatase; CRP: C-reactive protein.
* Independent T-test, ** Chi-square test; *** Accuracy test.
After three months of intervention, the average decrease in the FBS levels of the group taking nettle and bilberry was significantly higher than this value in the placebo-taking group (P < 0.001). Further, the reduction in the triglyceride level in the nettle-bilberry-taking group was 4.72 ± 4.48 units, representing a significant difference from the placebo-taking group (0.53 ± 3.49, P < 0.001). The combination of nettle and bilberry had the potential to lower the average cholesterol level by 8.90 ± 33.55 units in comparison to the reduction of the same parameter by 4.96 ± 3.81 units in the placebo-taking group (P < 0.001). The difference in high-density lipoprotein was not statistically different (P = 0.175), while the decrease in low-density lipoprotein (LDL) was considerably higher in the active intervention group (P < 0.001). Regarding the other parameters of the blood samples of the two understudy groups, including hemoglobin A1c (HbA1c), urea, blood urea nitrogen (BUN), Creatinine, aspartate transaminase (AST), alanine transaminase (ALT), alkaline phosphatase (ALP), C-reactive protein (CRP), insulin, and Homeostatic Model Assessment for Insulin Resistance (HOMA-IR), no difference was detectable (P > 0.05, Table 2).
Table 2.
Changes in Lipid Profile and Glycemic Parameters in the Understudy Groups Before and After Intervention
|
Variable
|
Stage
|
Grouping
|
P
Value for Changes
*
|
|
Intervention (n=29)
|
Placebo (n=30)
|
| FBS |
Before |
129.41 ± 37.58
123.00 (71 to 238) |
142.50 ± 39.31
137.50 (88 to 292) |
< 0.001 |
| After |
119.55 ± 37.40
113.00 (63 to 227) |
137.60 ± 39.75
133.50 (85 to 284) |
| Changes |
9.86 ± 5.01
10 (-5 to 18) |
4.90 ± 3.48
5 (-5 to 11) |
| HbA1C |
Before |
7.06 ± 0.62
7.04 (5.70 to 9.00) |
7.14 ± 0.75
7.16 (6.00 to 9.30) |
0.100 |
| After |
5.90 ± 0.82
5.92 (3.10 to 7.90) |
5.82 ± 1.02
5.86 (4.00 to 8.60) |
| Changes |
1.12 ± 0.55
1.10 (0.21 to 3.10) |
1.33 ± 0.36
1.33 (0.20 to 2.10) |
| Urea |
Before |
31.55 ± 4.13
31 (25 to 40) |
32.1 ± 4.78
32 (20 to 43) |
0.076 |
| After |
29.14 ± 3.30
29 (23 to 37) |
32.37 ± 4.89
32 (19 to 43) |
| Changes |
2.41 ± 4.90
4 (-10 to 9) |
-0.27 ± 4.64
0 (-11 to 11) |
| BUN |
Before |
14.79 ± 2.01
15 (11 to 19) |
14.73 ± 2.26
15 (9 to 20) |
0.333 |
| After |
16.31 ± 1.63
16 (13 to 20) |
15.73 ± 2.18
16 (9 to 20) |
| Changes |
-1.52 ± 2.89
-2 (-7 to 4) |
-1.00 ± 2.41
-1 (-6 to 5) |
| Creatinine |
Before |
0.72 ± 0.11
0.70 (0.54 to 1.00) |
0.76 ± 0.13
0.75 (0.53 to 1.10) |
0.826 |
| After |
0.69 ± 0.10
0.70 (0.42 to 0.87) |
0.73 ± 0.08
0.71 (0.60 to 1.00) |
| Changes |
0.04 ± 0.10
0 (-0.11 to 0.27) |
0.04 ± 0.08
0.04 (-0.12 to 0.19) |
| Triglyceride |
Before |
114.62 ± 46.24
114 (58 to 267) |
117.33 ± 29.68
114 (82 to 185) |
< 0.001 |
| After |
109.90 ± 44.86
106 (49 to 257) |
116.80 ± 29.51
109.5 (78 to 189) |
| Changes |
4.72 ± 4.48
6 (-3 to 10) |
0.53 ± 3.49
-0.5 (-4 to 7) |
| Cholesterol |
Before |
154.90 ± 37.73
155 (101 to 210) |
160.27 ± 37.93
162.5 (101 to 255) |
< 0.001 |
| After |
146.00 ± 38.73
145 (88 to 201) |
155.63 ± 37.42
155 (94 to 250) |
| Changes |
8.90 ± 3.55
10 (-1 to 13) |
4.63 ± 3.81
5 (-2 to 10) |
| HDL |
Before |
44.00 ± 4.93
44 (36 to 55) |
42.33 ± 4.44
43 (32 to 48) |
0.175 |
| After |
47.52 ± 9.32
47 (34 to 70) |
43.80 ± 6.05
45 (31 to 52) |
| Changes |
-3.52 ± 4.97
-3 (-15 to 5) |
-1.47 ± 2.27
-2 (-6 to 4) |
| LDL |
Before |
94.93 ± 29.41
97 (49 to 140) |
103.27 ± 22.14
101 (80 to 183) |
< 0.001 |
| After |
67.93 ± 31.29
74 (15 to 111) |
96.33 ± 21.45
93.5 (71 to 171) |
| Changes |
27.00 ± 7.95
28 (5 to 40) |
6.93 ± 2.69
7 (1 to 12) |
| AST |
Before |
20.86 ± 6.46
19 (13 to 32) |
18.00 ± 6.74
16 (10 to 35) |
0.205 |
| After |
19.24 ± 6.13
20 (8 to 30) |
17.33 ± 5.84
16 (10 to 35) |
| Changes |
1.62 ± 2.80
2 (-5 to 6) |
0.67 ± 3.44
1 (-6 to 8) |
| ALT |
Before |
19.31 ± 7.19
18 (11 to 38) |
21.37 ± 6.93
23 (12 to 37) |
0.825 |
| After |
17.97 ± 10.05
18 (3 to 43) |
20.30 ± 9.82
23 (5 to 38) |
| Changes |
1.34 ± 4.17
2 (-5 to 9) |
1.07 ± 4.18
1.5 (-8 to 10) |
| ALP |
Before |
147.21 ± 18.79
152 (108 to 174) |
154.97 ± 19.97
156 (125 to 185) |
0.584 |
| After |
142.97 ± 18.61
146.00 (110 to 171) |
150.43 ± 19.69
152.50 (120 to 180) |
| Changes |
4.24 ± 2.76
4 (-2 to 9) |
4.53 ± 3.08
4 (-8 to 10) |
| CRP |
Before |
2.82 ± 1.08
2.82 (1.20 to 4.53) |
2.37 ± 0.95
2.21 (1.14 to 4.71) |
0.110 |
| After |
2.32 ± 1.31
2.02 (1.00 to 5.10) |
2.49 ± 1.53
2.17 (1.00 to 6.44) |
| Changes |
0.50 ± 0.99
0.42 (-2.02 to 2.55) |
-0.12 ± 1.42
0.23 (-2.15 to 2.82) |
| Insulin |
Before |
13.72 ± 5.47
14.11 (5.20 to 21.47) |
14.52 ± 7.32
13.3 (2.32 to 33.62) |
0.564 |
| After |
18.57 ± 11.56
20.42 (1.45 to 36.89 |
19.08 ± 14.25
15.44 (1.02 to 57.38) |
| Changes |
-4.84 ± 6.16
-4.57 (-15.56 to 4.28) |
-4.57 ± 7.23
-4.10 (-23.76 to 4.70) |
| Insulin resistance (HOMAIR) |
Before |
2.73 ± 0.27
2.81 (2.23 to 3.25) |
2.83 ± 0.22
2.88 (2.26 to 3.16) |
0.328 |
| After |
2.90 ± 0.79
3.00 (1.58 to 5.33) |
3.24 ± 0.99
3.12 (1.07 to 6.30) |
| Changes |
-0.17 ± 0.81
-0.22 (-2.52 to 1.19) |
-0.41 ± 0.99
-0.25 (-3.32 to 1.40) |
Note. FBS: Fasting blood sugar; HbA1C: Hemoglobin A1C; BUN: Blood urea nitrogen; HDL: High-density lipoprotein; LDL: Low-density lipoprotein; AST: Aspartate aminotransferase; ALT: Alanine aminotransferase; ALP: Alkaline phosphatase; CRP: C-reactive protein.
*Mann-Whitney test.
Discussion
In the present study, the effects of a combination of nettle and bilberry were investigated in patients with T2DM. Based on our findings, after three months of intervention, evaluation of changes in FBS levels in the two understudy groups represented a significant difference, while this difference in the reduction of HbA1c was not statistically significant between the placebo and active intervention groups. It should be pointed out that this difference in kidney function tests (BUN, urea, and creatinine) was not statistically meaningful in our sample. In addition, regarding the liver function tests (LFTs), the average reduction in AST, ALT, and ALP, as well as the inflammation biomarkers (CRP), the difference was not statistically significant as well.
The currently utilized strategy to treat T2DM depends on a combination of insulin-stimulating and insulin-sensitizing drugs. Despite good glycemic control drugs at the beginning of treatment, their efficacy decreases over time. Furthermore, side effects such as severe hypoglycemia, lactic acidosis, idiosyncratic liver cell damage, GI discomfort, dizziness, and even death have been experienced by long-term use of these drugs and are considered the other drawbacks.5 Due to the high prevalence of DM in different societies and its complications, physicians and druggists have been looking for alternative treatment options, especially medicinal/herbal plants.17 The use of medicinal/herbal plants has been popular among people for a long time. Some of them have been proven to be effective and are considered complementary treatment options,18-20 while some others were found to be ineffective.21
Nettle leaves comprise flavonoids, peptides, and amines with anti-diabetic effects.7 These components take part in some mechanisms such as stimulating glycogenesis, closing potassium channels in pancreatic cells, and interfering with glucose absorption from the intestinal wall. Several studies have documented the positive effects of using nettle leaf extract or its other parts in the form of injection or oral use in treating DM.13
Vaccinium is a genus of shrubs with wide usage in herbal medicine. Cranberry is an effective and important medicinal plant in preventing inflammation, lowering blood lipids and glucose, decreasing oxidative stresses, preventing cardiovascular diseases, and treating dementia and other age-related diseases. There is also evidence of the antimicrobial properties of cranberry.22 Cranberry is well known for its anti-diabetes properties and through ages, different kinds of this fruit along with leaves have been used to improve diabetic symptoms.23 In a study on Italian herbal medicine, cranberry has been ranked fourth in the list of plants for controlling blood glucose.22 This study could not detect a significant anti-inflammatory effect for a nettle-bilberry product based on serum CRP levels.
In two studies conducted by Ghalavand et al23 and Ziaei et al,24 it was reported that consuming nettle supplements is an effective way to control blood sugar and high blood pressure in T2DM people. In our sample of T2DM patients, the average reduction in the level of insulin, as well as HOMA-IR, was not significantly different between the groups, while changes in FBS levels were different between the groups. The onset of T2DM disease is when the cells of the body are unable to produce and secrete enough insulin or to respond to insulin, which is known as resistance to insulin.1-3 In healthy people, insulin acts as a means to transport glucose into cells and signals them to take it up. Nonetheless, when insulin resistance is developed, cells become desensitized to this signaling. When resistance is developed in a noticeable number of cells, blood sugar and thus T2DM increase, which is usually called hyperglycemia.1,3
DM is associated with long-term damage and dysfunctions of various organs such as the retina (retinopathy), nerves (neuropathy), heart and blood vessels, and amputation.2 Moreover, poorly controlled T2DM can lead to multiple complications such as kidney failure and liver dysfunction.2,3 In our sample, this difference in kidney function tests (BUN, urea, and creatinine), as well as the LFT, including AST, ALT, and ALP, the difference was not statistically significant between the nettle-bilberry and placebo groups.
Bilberry and nettle are among the most commonly used medicinal plants in anti-diabetic formulas.25,26 A decoction of the combination of V. myrtillus and U. dioica leaves is widely employed in Russia as a blood glucose-lowering component. This binary combination has been found to reduce glycemia, enhance the utilization of glucose, protect pancreatic β-cells, inhibit intestinal glucose absorption, and show total cholesterol-lowering activity.27-30 The current study assessed the efficacy of this combination in T2DM patients, and the results revealed that it was effective in controlling FBS levels and cholesterol.
The present study was designed by considering the serious side effects of using hypoglycemic drugs, on the one hand, and the lack of significant side effects of the therapeutic doses of medicinal/herbal plants, including nettle and bilberry, on the other hand. The willingness and encouragement of physicians to use medicinal plants due to their wider and easy availability and the strong belief of people in the effectiveness of herbal medicine were also taken into account. The limited sample size as a single-center study was the main limitation of this study.
Conclusion
Overall, a combination of nettle and bilberry was effective in controlling FBS levels in patients with T2DM, while this production did not affect HbA1C levels in these patients. Nettle-bilberry intervention is similar to a placebo regarding kidney function, LFTs, and inflammation biomarkers, but this herbal product is effective in controlling cholesterol. There is a need for future studies on this topic to obtain more conclusive evidence.
Disclosure of funding source
This article is the result of a Ph.D. thesis, and financial support was provided by the Research Vice-chancellor of Tabriz University of Medical Sciences, Tabriz, Iran (Grant number: 64464).
Conflict of interests declaration
The authors declare that they have no known competing financial interests or personal relationships that could have influenced the work reported in this paper.
Acknowledgements
We would like to appreciate the cooperation of the Clinical Research Development Unit of Imam Reza General Hospital, Tabriz, Iran in conducting this research.
References
- Yahaya TO, Salisu TF. A review of type 2 diabetes mellitus predisposing genes. Curr Diabetes Rev 2019; 16(1):52-61. doi: 10.2174/1573399815666181204145806 [Crossref] [ Google Scholar]
- Adeshara KA, Diwan AG, Tupe RS. Diabetes and complications: cellular signaling pathways, current understanding and targeted therapies. Curr Drug Targets 2016; 17(11):1309-28. doi: 10.2174/1389450117666151209124007 [Crossref] [ Google Scholar]
- Hameed I, Masoodi SR, Mir SA, Nabi M, Ghazanfar K, Ganai BA. Type 2 diabetes mellitus: from a metabolic disorder to an inflammatory condition. World J Diabetes 2015; 6(4):598-612. doi: 10.4239/wjd.v6.i4.598 [Crossref] [ Google Scholar]
- Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract 2010; 87(1):4-14. doi: 10.1016/j.diabres.2009.10.007 [Crossref] [ Google Scholar]
- Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract 2018; 138:271-81. doi: 10.1016/j.diabres.2018.02.023 [Crossref] [ Google Scholar]
- Khatirnamani Z, Bakhshi E, Naghipour A, Hosseinzadeh S. Assessment of hemoglobin A1C in patients with type 2 diabetes in the first three years of care and its related factors. Journal of Health Promotion Management 2017; 6(5):34-42. doi: 10.21859/jhpm-07035.[Persian] [Crossref] [ Google Scholar]
- Moravej Aleali A, Amani R, Shahbazian H, Namjooyan F, Latifi SM, Cheraghian B. The effect of hydroalcoholic Saffron (Crocus sativus L) extract on fasting plasma glucose, HbA1c, lipid profile, liver, and renal function tests in patients with type 2 diabetes mellitus: a randomized double-blind clinical trial. Phytother Res 2019; 33(6):1648-57. doi: 10.1002/ptr.6351 [Crossref] [ Google Scholar]
- Varut RM, Gîrd CE, Rotaru LT, Varut MC, Pisoschi CG. Evaluation of polyphenol and flavonoid profiles and the antioxidant effect of Carduus acanthoides hydroalcoholic extract compared with Vaccinium myrtillus in an animal model of diabetes mellitus. Pharm Chem J 2018; 51(12):1088-95. doi: 10.1007/s11094-018-1746-0 [Crossref] [ Google Scholar]
- Avin M, Hasani-Ranjbar S, Larijani B, Abdollahi M. A systematic review of efficacy and safety of Urtica dioica in the treatment of diabetes. Int J Pharmacol 2011; 7(2):161-70. [ Google Scholar]
- Samakar B, Mehri S, Hosseinzadeh H. A review of the effects of Urtica dioica (nettle) in metabolic syndrome. Iran J Basic Med Sci 2022; 25(5):543-53. doi: 10.22038/ijbms.2022.58892.13079 [Crossref] [ Google Scholar]
- Namazi N, Tarighat A, Bahrami A. The effect of hydro alcoholic nettle (Urtica dioica) extract on oxidative stress in patients with type 2 diabetes: a randomized double-blind clinical trial. Pak J Biol Sci 2012; 15(2):98-102. doi: 10.3923/pjbs.2012.98.102 [Crossref] [ Google Scholar]
- Namazi N, Tarighat Esfanjani A, Avari M, Heshmati J. Effects of hydroalcoholic nettle extract on insulin sensitivity and some inflammatory indicator in type 2 diabetic patients. Avicenna J Clin Med 2012;18(4):10-4. [Persian].
- Amiri Behzadi A, Kalalian-Moghaddam H, Ahmadi AH. Effects of Urtica dioica supplementation on blood lipids, hepatic enzymes and nitric oxide levels in type 2 diabetic patients: a double blind, randomized clinical trial. Avicenna J Phytomed 2016; 6(6):686-95. [ Google Scholar]
- Chehri A, Yarani R, Yousefi Z, Shakouri SK, Ostadrahimi A, Mobasseri M. Phytochemical and pharmacological anti-diabetic properties of bilberries (Vaccinium myrtillus), recommendations for future studies. Prim Care Diabetes 2022; 16(1):27-33. doi: 10.1016/j.pcd.2021.12.017 [Crossref] [ Google Scholar]
- Asgary S, Rafieian Kopaei M, Sahebkar A, Shamsi F, Goli-Malekabadi N. Anti-hyperglycemic and anti-hyperlipidemic effects of Vaccinium myrtillus fruit in experimentally induced diabetes (antidiabetic effect of Vaccinium myrtillus fruit). J Sci Food Agric 2016; 96(3):764-8. doi: 10.1002/jsfa.7144 [Crossref] [ Google Scholar]
- Jakesevic M, Xu J, Aaby K, Jeppsson B, Ahrné S, Molin G. Effects of bilberry (Vaccinium myrtillus) in combination with lactic acid bacteria on intestinal oxidative stress induced by ischemia-reperfusion in mouse. J Agric Food Chem 2013; 61(14):3468-78. doi: 10.1021/jf400203h [Crossref] [ Google Scholar]
- Rezaeizadeh H, Alizadeh M, Naseri M, Shams Ardakani MR. The traditional Iranian medicine point of view on health and disease. Iran J Public Health 2009; 38(Suppl 1):169-72. [ Google Scholar]
- Yu X, Xu L, Zhou Q, Wu S, Tian J, Piao C. The efficacy and safety of the Chinese herbal formula, JTTZ, for the treatment of type 2 diabetes with obesity and hyperlipidemia: a multicenter randomized, positive-controlled, open-label clinical trial. Int J Endocrinol 2018; 2018:9519231. doi: 10.1155/2018/9519231 [Crossref] [ Google Scholar]
- Sadigi B, Yarani R, Mirghafourvand M, Travica N, Yousefi Z, Shakouri SK. The effect of saffron supplementation on glycemic parameters: an overview of systematic reviews. Phytother Res 2022; 36(9):3444-58. doi: 10.1002/ptr.7542 [Crossref] [ Google Scholar]
- Abdollahi A, Adelibahram F, Ghassab-Abdollahi N, Araj-Khodaei M, Parsian Z, Mirghafourvand M. The effect of Salvia officinalis on blood glycemic indexes and blood lipid profile in diabetic patients: a systematic review and meta-analysis. J Complement Integr Med. 2022. 10.1515/jcim-2021-0425.
- Jafarizadeh A, Raeisi SA, Ghassab-Abdollahi N, Yarani R, Araj-Khodaei M, Mirghafourvand M. Effect of Citrullus colocynthis on glycemic factors and lipid profile in type II diabetic patients: a systematic review and meta-analysis. J Diabetes Metab Disord 2022; 21(2):1785-95. doi: 10.1007/s40200-022-01045-9 [Crossref] [ Google Scholar]
- Benzie IF, Wachtel-Galor S. Herbal Medicine: Biomolecular and Clinical Aspects. Boca Raton, FL: CRC Press; 2011.
- Martineau LC, Couture A, Spoor D, Benhaddou-Andaloussi A, Harris C, Meddah B. Anti-diabetic properties of the Canadian lowbush blueberry Vaccinium angustifolium Ait. Phytomedicine 2006; 13(9-10):612-23. doi: 10.1016/j.phymed.2006.08.005 [Crossref] [ Google Scholar]
- Ziaei R, Foshati S, Hadi A, Hojati Kermani MA, Ghavami A, Clark CCT. The effect of nettle (Urtica dioica) supplementation on the glycemic control of patients with type 2 diabetes mellitus: a systematic review and meta-analysis. Phytother Res 2020; 34(2):282-94. doi: 10.1002/ptr.6535 [Crossref] [ Google Scholar]
- Sharafetdinov K, Kiseleva TL, Kochetkova AA, Mazo VK. Promising plant sources of anti-diabetic micronutrients. J Diabetes Metab 2017; 8(12):778. doi: 10.4172/2155-6156.1000778 [Crossref] [ Google Scholar]
- Shikov AN, Narkevich IA, Akamova AV, Nemyatykh OD, Flisyuk EV, Luzhanin VG. Medical species used in Russia for the management of diabetes and related disorders. Front Pharmacol 2021; 12:697411. doi: 10.3389/fphar.2021.697411 [Crossref] [ Google Scholar]
- El Haouari M, Rosado JA. Phytochemical, anti-diabetic and cardiovascular properties of Urtica dioica L (Urticaceae): a review. Mini Rev Med Chem 2019; 19(1):63-71. doi: 10.2174/1389557518666180924121528 [Crossref] [ Google Scholar]
- Golalipour MJ, Khori V. The protective activity of Urtica dioica leaves on blood glucose concentration and beta-cells in streptozotocin-diabetic rats. Pak J Biol Sci 2007; 10(8):1200-4. doi: 10.3923/pjbs.2007.1200.1204 [Crossref] [ Google Scholar]
- Bnouham M, Merhfour FZ, Ziyyat A, Mekhfi H, Aziz M, Legssyer A. Antihyperglycemic activity of the aqueous extract of Urtica dioica. Fitoterapia 2003; 74(7-8):677-81. doi: 10.1016/s0367-326x(03)00182-5 [Crossref] [ Google Scholar]
- Avci G, Kupeli E, Eryavuz A, Yesilada E, Kucukkurt I. Antihypercholesterolaemic and antioxidant activity assessment of some plants used as remedy in Turkish folk medicine. J Ethnopharmacol 2006; 107(3):418-23. doi: 10.1016/j.jep.2006.03.032 [Crossref] [ Google Scholar]