Int J Drug Res Clin. 2023;1:e6.
doi: 10.34172/ijdrc.2023.e6
Original Article
Investigation of the Frequency of Insulin Use Compared to Other Anti-diabetic Drugs in Diabetic Patients Presenting Acute Stroke
Masoumeh Poureskandari 1  , Samad Shams Vahdati 1, Elyar Sadeghi-Hokmabadi 1, Samad Gholzari 2, 3, Nahal Aghajamal 1, Alireza Ala 1, *
, Samad Shams Vahdati 1, Elyar Sadeghi-Hokmabadi 1, Samad Gholzari 2, 3, Nahal Aghajamal 1, Alireza Ala 1, * 
Author information:
1Emergency and Trauma Care Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
2Department of Anesthesiology and Intensive Care Medicine, Dortmund General Hospital, Dortmund, Germany
3Department of Health, Witten-Herdecke University, Witten, Germany
Abstract
Background:
This study aimed to measure the frequency of insulin use, compared to other antidiabetic drugs, in diabetic patients presenting with acute stroke in order to investigate its effect on the incidence of stroke.
Methods:
All diabetic patients with acute stroke who were referred to the emergency department within one year were included in this retrospective descriptive-analytic study. The collected data were statistically analyzed using SPSS 20. Data were reported as descriptive statistics (frequency and percentage) and means (±SD). Non-independent t test and chi-square test were used to compare quantitative and qualitative variables, respectively (P=0.05).
Results:
Out of 896 patients admitted to the stroke care unit, 191 cases were diagnosed with diabetes mellitus (DM). Computerized tomography (CT) scan findings performed in the emergency department represented about 30% of hemorrhagic results. There was a significant relationship between the type of diabetes treatment and the age of the patients, the CT scan findings, and the duration of DM in the patients.
Conclusion:
Therefore, patients with long-term involvement with diabetes and patients with high creatinine, due to insulin use, are discharged from hospitals with better conditions.
Keywords: Insulin, Hyperglycemic drugs, Stroke
Introduction
Cardiovascular disease (CVD), including stroke, is a serious health problem in both developing and developed countries and has detrimental effects on the person, family, and society.1
The most important modifiable risk factors for stroke are hypertension, diabetes, smoking, and dyslipidemia. Diabetes is a known risk factor for stroke. It can cause pathological changes in the blood vessels in different places and lead to a stroke if it directly affects the vessels in the brain. Additionally, with uncontrolled blood glucose levels in stroke patients, mortality is higher and post-stroke outcomes are worse.2
A meta-analysis of studies has shown that the ratio of ischemic strokes in people with diabetes, compared to people without diabetes, is 2.27.3 Furthermore, diabetes may be accountable for more than 8% of first ischemic strokes. In addition, strokes are worse in diabetic patients, leading to increased mortality and disability.4 Thus, stroke prevention in these patients has become an important issue. It can be highly useful to know if one diabetes drug is more protective against stroke than another. However, until lately, no oral agent drugs (OAD) have been approved to reduce the incidence or recurrence of stroke, and lowering blood glucose has been generally disappointing in terms of cardiovascular protection associated with diabetes.5,6 There is still hope that OAD may provide cardiovascular advantages impartial to glycemic control.
Based on the above-mentioned explanation, this study sought to measure the frequency of insulin use, compared to other OADs, in diabetic patients presenting with acute stroke in order to evaluate its effect on the incidence of stroke.
Methods
This was a descriptive-retrospective study.
Method of Implementation
All diabetic patients with acute stroke who were referred to the emergency department within one year were included in the current study. The size of the sample was numerically based on the stroke registry documentation. Patients under the age of 18, who either left the hospital before completing treatment or had incomplete records, and those who received combined treatment of insulin and OAD were excluded from the study. The variables of interest, including age, gender, creatinine serum level, risk factors, imaging findings, use of insulin or pills, duration of diabetes, and outcomes were entered in the researcher-made checklist.
Statistical Analysis
The collected data were statistically analyzed using SPSS statistical analysis software, version 20.0 (Microsoft LTD, Chicago, USA). Data were reported as descriptive statistics (frequency and percentage) and means ( ± standard deviation). Non-independent t test and chi-square test were employed to compare quantitative and qualitative variables, respectively, and a P value of less than 0.05 was considered for statistical significance.
Results
Overall, 896 patients, including 99 (51.8%) males and 92 (48.2%) females, were admitted to the stroke care unit with a diagnosis of stroke during 2017-2018; out of these cases, 191 patients were known to have diabetes mellitus (DM). Based on the Kolmogorov-Smirnov statistical test, age did not follow a normal distribution (P = 0.01).
The mean age and the median age of patients (67.70-84.84) were 69.34 ± 10.56 years and 71 years, respectively. The minimum and maximum age range was 38 and 91 years, respectively.
Emergency brain computerized tomography (CT) scan findings showed nearly 29% of hemorrhagic findings and 33% of ischemic strokes (Figure 1).
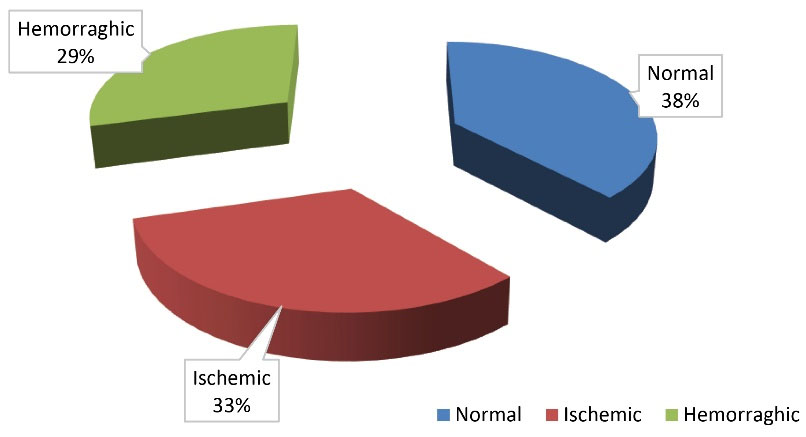
Figure 1.
Frequency of Brain CT Scan Findings. Note. CT: Computerized tomography
.
Frequency of Brain CT Scan Findings. Note. CT: Computerized tomography
Among these patients, 19 (9.9%) and 172 (90.1%) cases were treated with insulin and controlled with OAD, respectively.
The average duration of the known diabetes of patients was 7.32 ± 2.96 years with a minimum of 1 year and a maximum of 22 years with a median of 7 years. In the range of 25-75%, this number was between 5 and 9 years.
The average creatinine serum level of the patients was 1.25 ± 0.37 mmol/dL with a minimum of 1 and a maximum of 2 mmol/dL. This number was between 1.05 and 1.30 mmol/dL in the range between 25% and 75%.
In the study of complications admitted to the stroke care unit, the most common complications were urinary tract infection and sepsis, followed by aspiration pneumonia (Table 1).
Table 1.
Frequency of Hospitalization Complications of Stroke Patients With a History of Diabetes
|
Side Effect
|
Frequency
|
Percent
|
| Aspiration pneumonia |
32 |
16.8 |
| Deep vein thrombosis |
4 |
2.1 |
| Pulmonary emboli |
4 |
1.2 |
| Urinary infectious disease |
63 |
33 |
| Sepsis |
41 |
21.5 |
| Bedsore |
18 |
9.4 |
| Myocardial infarction |
4 |
2.1 |
| Gastrointestinal bleeding |
6 |
3.1 |
| Seizure |
8 |
4.2 |
The baseline factor was adjusted for comparing the variables between the two groups of insulin treatment and antidiabetic oral agent groups (e.g., age, gender, comorbidity, and the like). A significant relationship was observed between the type of diabetes treatment and the age of patients, which was a weak relationship (P < 0.001, R2 = 0.296).
Further, a significant relationship was found between the type of diabetes treatment and the CT scan findings of the patients, which was negligible (P = 0.031, R2 = 0.156).
Moreover, there was a significant relationship between the type of diabetes treatment and the history of hypertension of patients, which was a weak and inverse relationship (P = 0.001, R2 = -0.243).
The results further revealed a significant relationship between the type of diabetes treatment and the duration of DM in patients, which was moderate and inverse (P < 0.001, R2 = -0.326).
Moreover, a significant relationship was observed between the type of diabetes treatment and patients’ creatinine serum level, which was relatively strong and inverse (P < 0.001, R2 = - 0.715).
Based on the findings, there was a significant relationship between the type of diabetes treatment and the discharge conditions of the patients, which was a weak relationship (P = 0.049, R2 = 0.143).
The results demonstrated a significant relationship between the duration of diabetes treatment and the gender of patients, which was a weak relationship (P = 0.049, R2 = 0.143).
Finally, a significant relationship was found between the duration of diabetes treatment and patients’ creatinine serum level, which was also weak (P < 0.001, r = 0.279).
Discussion
The main goal of diabetes management is to achieve and maintain a certain blood sugar level.7 The significance of controlling the glucose level in the reduction of vascular consequences is well recognized.8 However, the development of new methods in the treatment of diabetes and attention to the safety profile of common treatments has led to a debate about the optimal target level.9-11 In type 2 diabetes mellitus (T2DM), metformin monotherapy is recommended in the case of failure in diet and exercise.12 Adding a sulfonylurea to the regimen or, if contraindicated, adding a dipeptidyl peptidase-4 inhibitor or a thiazolidinedione is recommended if metformin monotherapy does not work. Exogenous insulin is one of the most well-known therapeutic methods for reducing blood sugar, and in recent years, it has become more popular in people with T2DM.13 There are several mechanisms that may cause adverse vascular events in T2DM cases who take exogenous insulin, including cardiac arrhythmias due to hypoglycemia,14 vascular inflammation,15 and blood coagulation.16 At the same time, the relationship between insulin therapy and cancer is under considerable scrutiny. The results of some studies support a reduction in the risk of cancer outcomes associated with the use of metformin compared to sulfonylurea monotherapy.17,18 Recent data have indicated that at the start of insulin therapy in Europe, the average hemoglobin A1c (HbA1c) is approximately 10%.19 Currie et al conducted a study on the outcomes of insulin treatment and other OAD treatments in T2DM and concluded that the risk of diabetes-related complications such as cardiovascular events, neuropathy, eye problems, stroke, renal failure, cancer, and all-cause mortality was higher in insulin treatment compared to metformin therapy.20 Of course, other individual characteristics between these two treatment groups should also be taken into consideration.
In a meta-analysis performed by Li et al, it was found that in a comparison between OADs used to lower blood glucose and insulin, insulin may reduce the risk of heart failure in diabetic patients, but this effect was only noticeable in patients who had no previous CVD and were not at high risk for it, while it was not observed in the other groups. Nonetheless, insulin did not affect the risk of mortality and other cardiovascular outcomes.21
According to these findings, physicians should consider the benefits and defects when prescribing insulin therapy. Treatment with insulin has many drawbacks, including discomfort (injections and close monitoring of blood sugar), the possibility of excessive blood sugar drop, and gaining weight. Therefore, they concluded that there is currently no strong evidence to support insulin therapy for this society.
Unlike the previous study, Anyanwagu et al stated that recent large epidemiologic studies have reported increased adverse cardiovascular outcomes and mortality with insulin therapy, compared with non-insulin therapy, in T2DM, but they found no significant difference in the risk of death and cardiovascular events between the groups treated with insulin and non-insulin drugs. In their study, insulin showed greater effectiveness in controlling blood sugar, but the ratio of achieving the desired HbA1c level was similar in both groups. When using insulin, the probability of hypoglycemia was almost twice of the group without insulin, and this group did not have a significant change in the patient’s weight. Non-insulin OAD had more adverse effects.22 Rados et al reported that in T2DM cases, insulin therapy did not increase the risk of CVDs or mortality rate.23
Herman et al found that in the treatment of T2DM, the use of insulin may cause cardiovascular events, weight gain, hyperinsulinemia, or excessive hypoglycemia. They suggested that insulin should be reduced to lower stages in the treatment of T2DM; it should be used only when it is necessary, and there is no result from other drugs. Drugs that reduce the risk of vascular events and mortality and do not cause weight gain should be prioritized for treatment.24 In our study, a significant relationship was observed between the type of diabetes treatment and the age of the patients, and the relationship was weak. The probability of using insulin was higher when the patient was older, but this relationship was not strong. Additionally, a significant relationship was found between the type of diabetes treatment and the CT scan findings of the patients, and the relationship was weak. Similar to diabetic patients, using insulin had a higher probability of non-hemorrhagic findings in CT scans, but this relationship was not strong. In the present study, there was a significant relationship between the type of diabetes treatment and the duration of DM in patients, and the relationship was moderate and inverse. In other words, the probability of using insulin was higher when the duration of diabetes was longer.
Conclusion
According to the findings of this study, patients taking insulin had a better outcome and lower disability than patients who took OAD, and despite having a high serum creatinine level, which is probably the reason for taking insulin, they could experience better outcomes after discharge. Therefore, patients with long-term involvement with diabetes and those with a high creatinine serum level, due to insulin use, were discharged from hospitals with better conditions.
Ethics statement
The Ethics Committee of Tabriz University of Medical Sciences approved this study with registry No IR.TBZMED.REC.1399.319.
Disclosure of funding source
There was no specific grant from a public, commercial, or not-for-profit funding agency for conducting this research.
Conflict of interests declaration
None.
Acknowledgments
Special thanks to all emergency department staffs
Data availability statement
The data supporting this research will be available upon a reasonable request.
References
- Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation 2011; 123(8):933-44. doi: 10.1161/CIR.0b013e31820a55f5 [Crossref] [ Google Scholar]
- O’Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet 2010; 376(9735):112-23. doi: 10.1016/s0140-6736(10)60834-3 [Crossref] [ Google Scholar]
- Emerging Risk Factors Collaboration. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies The lancet. 2010 Ju n 26; 375(9733):2215-22. doi: 10.1016/S0140-6736(10)60484-9 [Crossref] [ Google Scholar]
- Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2014; 45(7):2160-236. doi: 10.1161/str.0000000000000024 [Crossref] [ Google Scholar]
- Laakso M. Cardiovascular disease in type 2 diabetes from population to man to mechanisms: the Kelly West Award Lecture 2008. Diabetes Care 2010; 33(2):442-9. doi: 10.2337/dc09-0749 [Crossref] [ Google Scholar]
- Azimova K, San Juan Z, Mukherjee D. Cardiovascular safety profile of currently available diabetic drugs. Ochsner J 2014; 14(4):616-32. [ Google Scholar]
- National Institute for Clinical Excellence. Type 2 Diabetes: The Management of Type 2 Diabetes. 2008. http://guidance.nice.org.uk/CG66. Accessed August 8, 2012.
- Sarwar N, Sattar N, Gudnason V, Danesh J. Circulating concentrations of insulin markers and coronary heart disease: a quantitative review of 19 Western prospective studies. Eur Heart J 2007; 28(20):2491-7. doi: 10.1093/eurheartj/ehm115 [Crossref] [ Google Scholar]
- Yudkin JS, Richter B, Gale EA. Intensified glucose lowering in type 2 diabetes: time for a reappraisal. Diabetologia 2010; 53(10):2079-85. doi: 10.1007/s00125-010-1864-z [Crossref] [ Google Scholar]
- European Medicines Agency. European Medicines Agency Update on Ongoing Benefit-Risk Review of Avandia, Avandamet and Avaglim. 2010. http://www.ema.europa.eu/docs/en_GB/document_library/Press_release/2010/07/WC500094981.pdf. Accessed August 5, 2012.
- FDA. FDA Drug Safety Communication: Ongoing Safety Review of Actos (Pioglitazone) and Potential Increased Risk of Bladder Cancer After Two Years Exposure. 2010. Available from: http://www.fda.gov/Drugs/Drugsafety/ucm226214.htm. Accessed August 5, 2012.
- Nathan DM, Buse JB, Davidson MB, Ferrannini E, Holman RR, Sherwin R. Medical management of hyperglycaemia in type 2 diabetes mellitus: a consensus algorithm for the initiation and adjustment of therapy. Diabetologia 2009; 52(1):17-30. doi: 10.1007/s00125-008-1157-y [Crossref] [ Google Scholar]
- Currie CJ, Peters JR, Evans M. Dispensing patterns and financial costs of glucose-lowering therapies in the UK from 2000 to 2008. Diabet Med 2010; 27(7):744-52. doi: 10.1111/j.1464-5491.2009.02849.x [Crossref] [ Google Scholar]
- Nordin C. The case for hypoglycaemia as a proarrhythmic event: basic and clinical evidence. Diabetologia 2010; 53(8):1552-61. doi: 10.1007/s00125-010-1752-6 [Crossref] [ Google Scholar]
- Antoniades C, Tousoulis D, Marinou K, Papageorgiou N, Bosinakou E, Tsioufis C. Effects of insulin dependence on inflammatory process, thrombotic mechanisms and endothelial function, in patients with type 2 diabetes mellitus and coronary atherosclerosis. Clin Cardiol 2007; 30(6):295-300. doi: 10.1002/clc.20101 [Crossref] [ Google Scholar]
- Angiolillo DJ, Bernardo E, Ramírez C, Costa MA, Sabaté M, Jimenez-Quevedo P. Insulin therapy is associated with platelet dysfunction in patients with type 2 diabetes mellitus on dual oral antiplatelet treatment. J Am Coll Cardiol 2006; 48(2):298-304. doi: 10.1016/j.jacc.2006.03.038 [Crossref] [ Google Scholar]
- Bowker SL, Yasui Y, Veugelers P, Johnson JA. Glucose-lowering agents and cancer mortality rates in type 2 diabetes: assessing effects of time-varying exposure. Diabetologia 2010; 53(8):1631-7. doi: 10.1007/s00125-010-1750-8 [Crossref] [ Google Scholar]
- Currie CJ, Poole CD, Gale EA. The influence of glucose-lowering therapies on cancer risk in type 2 diabetes. Diabetologia 2009; 52(9):1766-77. doi: 10.1007/s00125-009-1440-6 [Crossref] [ Google Scholar]
- Liebl A, Jones S, Benroubi M, Castell C, Goday A, Aline Charles M. Clinical outcomes after insulin initiation in patients with type 2 diabetes: 6-month data from the INSTIGATE observational study in five European countries. Curr Med Res Opin 2011; 27(5):887-95. doi: 10.1185/03007995.2011.555755 [Crossref] [ Google Scholar]
- Currie CJ, Poole CD, Evans M, Peters JR, Morgan CL. Mortality and other important diabetes-related outcomes with insulin vs other antihyperglycemic therapies in type 2 diabetes. J Clin Endocrinol Metab 2013; 98(2):668-77. doi: 10.1210/jc.2012-3042 [Crossref] [ Google Scholar]
- Li J, Tong Y, Zhang Y, Tang L, Lv Q, Zhang F, et al. Effects on all-cause mortality and cardiovascular outcomes in patients with type 2 diabetes by comparing insulin with oral hypoglycemic agent therapy: a meta-analysis of randomized controlled trials. Clin Ther 2016;38(2):372-86.e6. 10.1016/j.clinthera.2015.12.006.
- Anyanwagu U, Mamza J, Donnelly R, Idris I. Comparison of cardiovascular and metabolic outcomes in people with type 2 diabetes on insulin versus non-insulin glucose-lowering therapies (GLTs): a systematic review and meta-analysis of clinical trials. Diabetes Res Clin Pract 2016; 121:69-85. doi: 10.1016/j.diabres.2016.09.002 [Crossref] [ Google Scholar]
- Rados DV, Falcetta MRR, Pinto LC, Leitão CB, Gross JL. All-cause mortality and cardiovascular safety of basal insulin treatment in patients with type 2 diabetes mellitus: a systematic review with meta-analysis and trial sequential analysis. Diabetes Res Clin Pract 2021; 173:108688. doi: 10.1016/j.diabres.2021.108688 [Crossref] [ Google Scholar]
- Herman ME, O’Keefe JH, Bell DSH, Schwartz SS. Insulin therapy increases cardiovascular risk in type 2 diabetes. Prog Cardiovasc Dis 2017; 60(3):422-34. doi: 10.1016/j.pcad.2017.09.001 [Crossref] [ Google Scholar]