Int J Drug Res Clin. 2023;1:e11.
doi: 10.34172/ijdrc.2023.e11
Review Article
What is the Best Management for Geriatric Epistaxis? A Comprehensive Systematic Review and Meta-analysis
Kavous Shahsavarinia 1, 2  , Gholamreza Faridaalaee 2
, Gholamreza Faridaalaee 2  , Razaagh Eisazadeh Ahranjani 2, Moloud Balafar 2, Nooshin Milanchian 3
, Razaagh Eisazadeh Ahranjani 2, Moloud Balafar 2, Nooshin Milanchian 3  , Sakineh Hajebrahimi 4, Hanieh Salehi-Pourmehr 4, *
, Sakineh Hajebrahimi 4, Hanieh Salehi-Pourmehr 4, * 
Author information:
1Road Traffic Injury Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
2Emergency and Trauma Care Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
3Islamic Azad University of Tabriz Medical Sciences, Tabriz, Iran
4Research center for Evidence-Based Medicine, Iranian EBM Center: A Joanna Briggs Institute Center of Excellence, Tabriz University of Medical Sciences, Tabriz, Iran
Abstract
Background:
Given the importance of epistaxis in elder patients, this systematic review was conducted to determine the best non-surgical treatment of epistaxis in elder patients.
Methods:
A systematic search of references was performed to investigate non-surgical methods in administering epistaxis in elder people in March 2022 for relevant articles.
Results:
Among 1613 retrieved articles in the initial search, 28 studies were included, and the mean re-bleeding in 18 studies was 18%. Regarding the treatment methods, 35.7%, 14.3%, 10.7%, and 10.7% used nasal packing, intranasal topical tranexamic acid, silver nitrate, and Floseal® treatment, respectively. The highest success rate was related to topical tranexamic acid compared to topical oxymetazoline spray (Odds ratio [OR]: 6.50, 95% confidence interval [CI]: 1.54-27.49, P=0.011), followed by nasal compression with tranexamic acid compared to the placebo.
Conclusion:
It seems that tranexamic acid has a beneficial effect on controlling epistaxis in the elderly. However, well-designed large randomized controlled trials are indicated for an accurate conclusion.
Keywords: Epistaxis, Geriatrics, Systematic review
Introduction
Despite the fact that 60% of people encounter epistaxis at least once in their lives and epistaxis is one of the most frequently occurring disorders, only 6% of people who experience nosebleeds seek medical assistance.1-3 Epistaxis occurs when the mucus is worn away, and the vessels are damaged and ruptured subsequently. Although epistaxis annoys most people in the community, most of these bleedings are benign and self-limiting. However, this issue can occasionally be fatal, especially for elderly people and those who already have a serious illness. Based on the location of the bleeding, epistaxis can be categorized into anterior and posterior types.4 The tiny area (where the Kiesselbach’s plexus is formed on the septum) is the source of more than 90% of the anterior bleedings. Most commonly occurring in the posterior nasal cavity, the posterior epistaxis frequently has an arterial origin. Aspiration is more likely and its management is typically severe and difficult. The causes of epistaxis can be categorized into local, systemic, or idiopathic. Local causes include trauma, mucosal irritation, abnormalities of the nasal septum, inflammatory illnesses, and tumours. Systemic causes are blood dyscrasias, arteriosclerosis, and hereditary hemorrhagic telangiectasia. The most frequent cause is local nasal trauma, which is followed by facial trauma, foreign objects, sinus or nasal infections, and prolonged dry air inhalation.5
The age distribution is more on both ends of the age spectrum and more prevalent in young children (2-10 years) and elder people (50-80 years).6 In addition, in elder people, posterior epistaxis is more prevalent, occurs more severely, and requires more measures to control the bleeding.7 The recommended measures to control and treat epistaxis include surgical and non-surgical approaches. Non-surgical measures are the use of local decongestants (e.g., oxymetazoline), anesthetics (e.g., 4% lidocaine), antibiotic ointments that prevent infection at the injury site and moisturize the nasal environment (including 2% mupirocin ointment), blood coagulants (e.g., silver nitrate, which also has an antibacterial effect), use of hot water, as well as anterior and posterior nasal packing. Surgical measures include cauterization, arterial embolization, vascular ligature, or other methods.6,8,9 Most epistaxis can be cured with nasal tampons or cautery, but posterior epistaxis, which is frequently detected in elder people, is associated with pathology. Further, it puts the patient at risk and requires hospital admission and treatment. Since elder patients have comorbidity and their condition deteriorates due to epistaxis, they need fast treatment and special attention.10 Given the importance of epistaxis in elder patients, which can be life-threatening, and the lack of a single treatment guideline for these patients, a systematic study was conducted to review previous studies in this area with the hope of determining the best single approach in the non-surgical treatment of epistaxis in the elder patients.
Methods
Search Strategy and Selection Criteria
A systematic search of references was performed to investigate non-surgical methods in the control of epistaxis in elder people. Medline, Science Direct, Scopus, Ovid, ProQuest, Google Scholar, and Web of Science databases were searched until March 2022 for relevant articles. Relevant references in the selected studies were searched manually. Unpublished studies (grey literature) and studies presented at conferences were searched as well. Correspondence was performed with authors who were active in the area of the study topic to obtain information about published and unpublished studies. The following keywords were used to search for articles (Supplementary File 1):
Keywords: Elder patients, Epistaxis, and Nonsurgical management
Research definition of Population, Intervention, Comparison, and Outcome (PICO):
P: Elder Patients With Epistaxis
I: Nonsurgical Method
C: No Comparison Between the Methods
O: Re-bleeding
Inclusion Criteria
Studies that met the defined PICO.
Exclusion Criteria
Studies that were conducted on animal samples, reported no sample size, were non-English, and had no required quality. Two researchers independently reviewed the extracted studies according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. After duplicate identification and elimination, the remaining studies’ titles and abstracts were examined before examining the entire texts of the remaining studies. Conflicts over the screening and selection of research were settled by consensus or the judgement of a third party. This process was managed by utilizing Endnote 9 software.
Screening, Choosing, and Evaluating the Risk of Bias
One of the researchers assessed the papers’ quality, and a second researcher conducted ad hoc reevaluations using the JBI Critical Appraisal Checklist for Case Reports.
Data Extraction
Using the data extraction table created, based on the objectives, by one of the researchers and random evaluation by another researcher, data were extracted from the entered studies. The year, author, nation, study period, study kind, number of samples, mean age, male-to-female ratio, result, medicine type, and side effects were the collected data (Supplementary File 2).
Data Synthesis and Analysis
Cochran’s (Q) and I2 statistics, which show the percentage of changes between studies, were used to assess the heterogeneity between studies. The Mantel-Haenszel fixed effects model was employed if the I2 statistic value was less than 50%, and the random effects model was applied if it was greater than 50% or had a P value of 0.05. Comprehensive Meta-Analysis Software (version 2.0) was utilized for the statistical analysis, and a P value of 0.05 or less was regarded as significant.
Results
Descriptive of the Included Studies
A total of 1613 articles were found after a thorough scan of the references. Due to duplication, a total of 560 papers were eliminated from the study; additionally, 1008 articles were deleted after screening their titles and abstracts. Further, 17 publications were removed from the study after reading the entire texts of the papers. Finally, this meta-analysis study comprised 28 studies6,9,11-34 (Figure 1). The mean age of the study population was 68.13 (6.52) years, with a minimum age of 61 years and a maximum age of 84 years, according to the studies included in 24 of the papers. Based on the 16 articles that entered the study, 56.6% of the subjects were males and 43.4% were females. The mean re-bleeding rate in 18 studies was 18%. With regard to the risk factors, out of 28 studies, hypertension (HTN) was reported in 21 studies, and HTN was accompanied by diabetes mellitus (DM) in 7 of these cases (33%). In terms of the treatment methods, based on the information extracted from these studies, 35.7%, 14.3%, 10.7%, and 10.7% used nasal packing, intranasal topical tranexamic acid, silver nitrate, and Floseal® treatment, respectively. In 11 of these studies, the mean rate of reported mortality was 9.5%.

Figure 1.
Study Flow Diagram.
.
Study Flow Diagram.
Among the 13 studies, the percentage of cases that required hospitalization was 46%. In half of these studies, the mean time to stop bleeding was reported at 19 minutes, and the median was reported at 15 minutes (The minimum and maximum times were 5 minutes and one hour, respectively).
Meta-analysis Results
Based on data analysis, it was found that the most used treatment was related to the use of tranexamic acid, oral, topical, or nasal compression. Other treatment methods included rapid rhino nasal tampon and pneumatic tamponade, which had similar effects compared to placebo, rapid rocket nasal tampon, and nasal packing with Vaseline gauze. The results of the study revealed that the highest success rate was associated with topical tranexamic acid compared to topical oxymetazoline spray (odds ratio [OR]: 6.50, 95% confidence interval [CI]: 1.54-27.49, P = 0.011), followed by nasal compression with tranexamic acid compared to placebo (OR: 4.16, 95% CI: 1.24-13.99, P = 0.021). On the other hand, in comparison to nasal packing, the treatment with Floseal® homeostatic agent and tranexamic acid nasal compression had the lowest success rate. In addition, pneumatic tamponade had a lower success rate than choanal balloon tamponade (Figures 2-4 and Supplementary file 3).
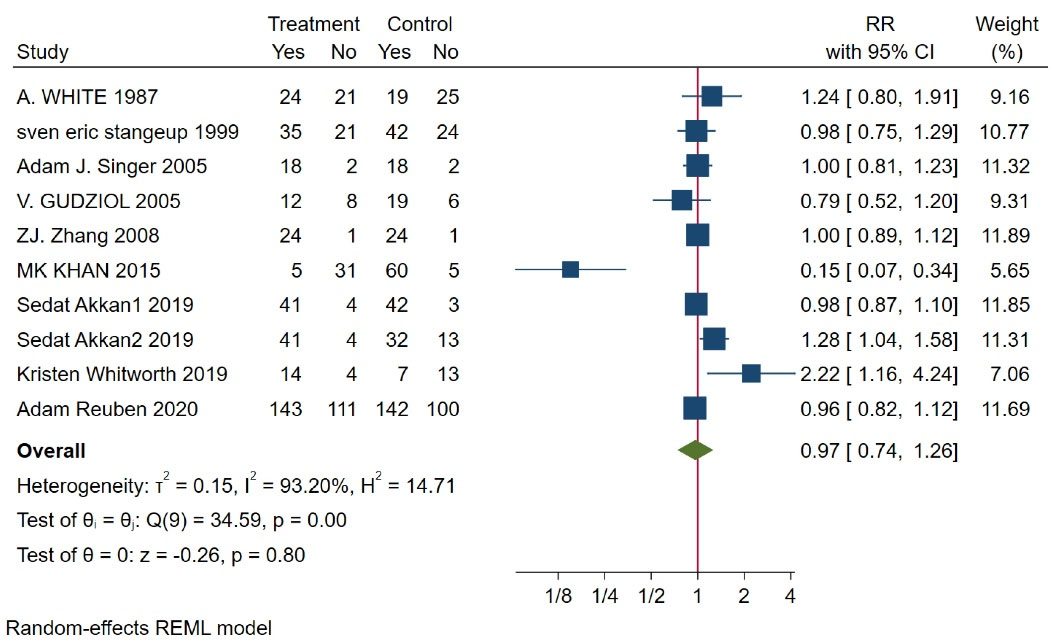
Figure 2.
Risk Ratio of the Effect of All Interventions in Comparison With Routine Management on Re-bleeding.
.
Risk Ratio of the Effect of All Interventions in Comparison With Routine Management on Re-bleeding.
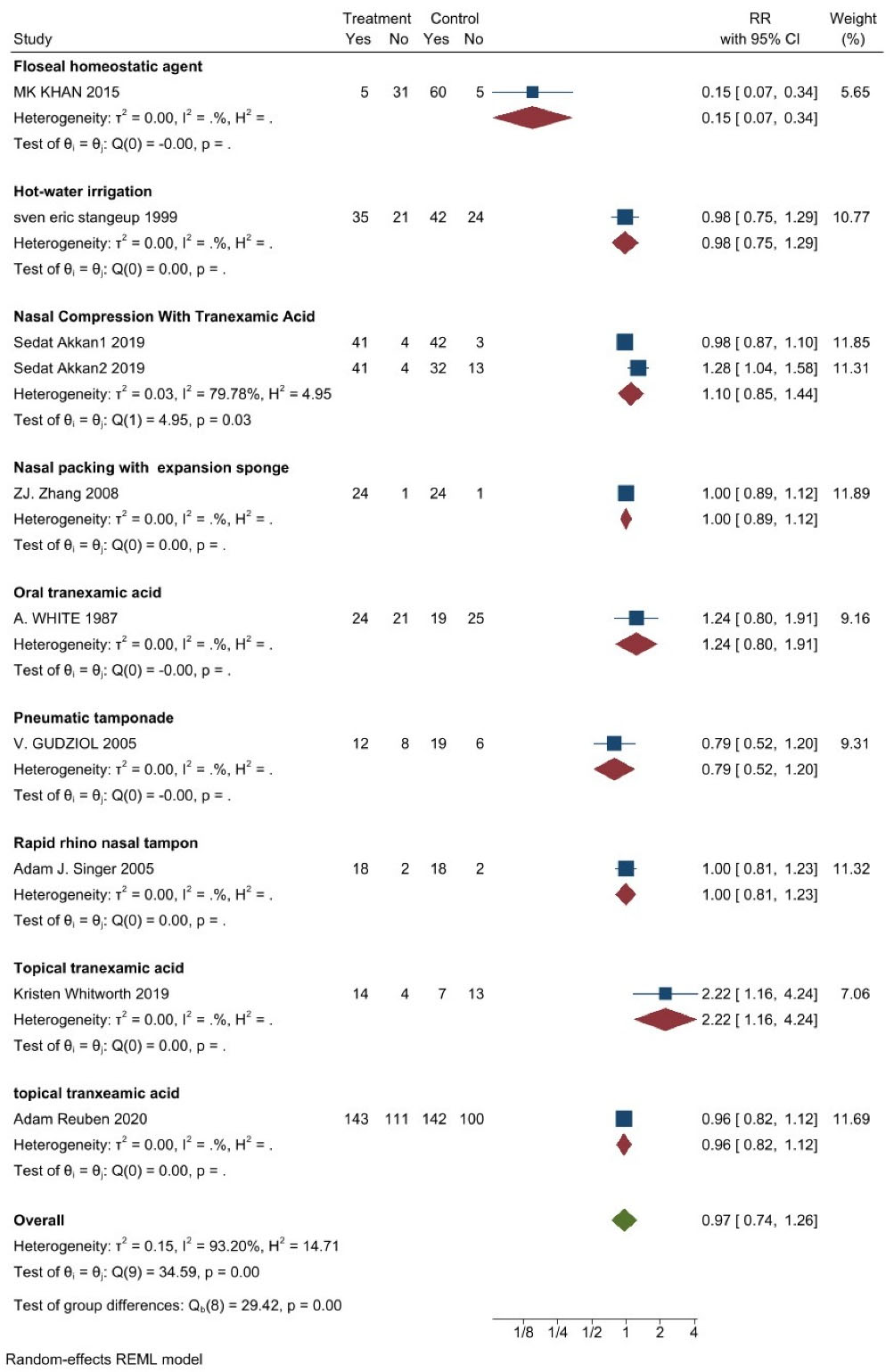
Figure 3.
The Risk Ratio of Different Therapeutic Approch in the Control of Re-bleeding.
.
The Risk Ratio of Different Therapeutic Approch in the Control of Re-bleeding.
Figure 4.
The Subgroup Analysis for the Risk Ratio of Re-bleeding.
.
The Subgroup Analysis for the Risk Ratio of Re-bleeding.
Heterogeneity
After reviewing 10 studies, the heterogeneity value was obtained, indicating the existence of serious heterogeneity in the studies. Meta-regression represented that the number of sample size in the studies and the ratio of gender and re-bleeding had a P value greater than 0.05, implying that these variables are not a significant source of heterogeneity. Although the number of studies was small, the drawn Begg’s test and Egger’s test, and sharp Funnel graph indicated the absence of publication bias (Figure 5).
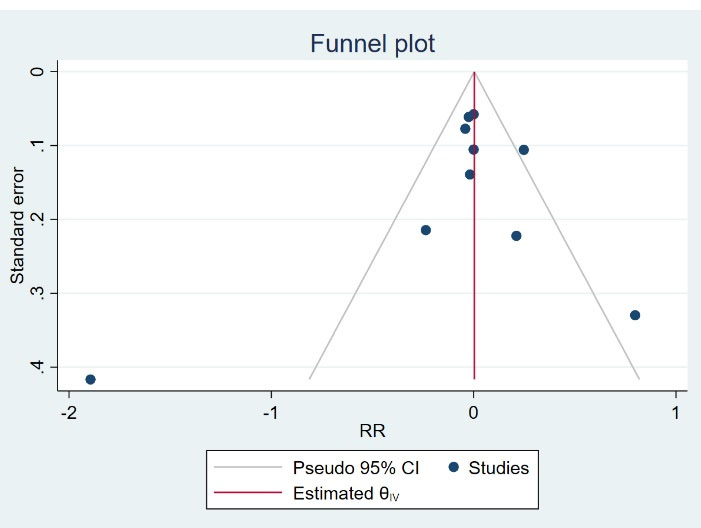
Figure 5.
Publication Bias.
.
Publication Bias.
Discussion
Older patients are more likely to experience posterior epistaxis. Epistaxis can cause mortality and morbidity in individuals with additional systemic diseases and susceptible populations, including children and the elderly. Epistaxis is caused by the combination of numerous local and systemic variables. These elements harm the nasal mucosa, have an impact on the vascular system, and/or hinder blood clotting. Systemic variables such as HTN, aging, and bleeding disorders are the most frequent causes of significant epistaxis in elderly people. Epistaxis is a result of vascular wall alterations brought on by aging, including arterial tunica media fibrosis. Therefore, older patients are more likely to experience epistaxis.35-37
Patients with epistaxis had a 24-64% prevalence of HTN according to reports.38,39 Controlled research has verified the link between HTN and epistaxis.
However, there was no evidence of an independent relationship between the severity of epistaxis and HTN in a cross-sectional investigation of hypertensive patients.40 Epistaxis can occasionally be a life-threatening emergency, particularly in elderly people with HTN and heavy bleeding.6 The findings of the current study are consistent with those of the previously cited studies on the risk factors of epistaxis, which identified HTN with or without DM as the primary risk factor.
In terms of the methods used in the treatment of epistaxis, according to the information extracted from these studies, 35.7%, 14.3%, 10.7%, and 10.7% utilized nasal packing, intranasal topical tranexamic acid, silver nitrate, and Floseal® treatment, respectively. Furthermore, the results of this study showed that the mean mortality was 9.5%, and 46% needed hospitalization.
Topical oxymetazoline spray may be beneficial in addition to compression in the control of epistaxis. This substance promotes vasoconstriction and alpha-adrenergic receptor stimulation.41,42 In one trial, 65% of individuals with epistaxis who went to the emergency room had their bleeding halted with oxymetazoline spray.10
Finding the bleeding point is the first step in treating acute epistaxis. Chemical or electrical cautery might be employed after locating the bleeding area. For small bleeding, especially, silver nitrate can be applied as a chemical caustic agent with little discomfort. Electrical cauterization should be utilized if there is significant anterior septal hemorrhage. Cauterization should be unilateral to avoid septum perforation.43 There is no evidence of the superiority of electrocautery to silver nitrate cautery.44
There are several different packing options, including anterior and posterior packs, which are both absorbable and non-absorbable. Oxidized cellulose such as Surgicel and gelatin foams such as Gelfoam are two common absorbable materials used for anterior packing. Floseal®, for instance, is a product that contains both thrombin and gelatin and is employed as a high-viscosity gel. Floseal® is a biodegradable matrix hemostatic sealant with two main components. Bovine-derived gelatin particles in the first component swell to create a tamponade action and a framework for platelet aggregation. Human-derived thrombin, the second component, speeds up clot formation. Because of its hemophilic characteristics, Floseal® can adhere to both wet and uneven surfaces effectively and quickly, halting bleeding on mucosal surfaces.45 These absorbable products are all simple to apply and painless. Other non-absorbable packaging supplies include air balloons, calcium alginate, polyvinyl alcohol (e.g., Merocel), and gauze soaked with petrolatum.46 The need to remove the material and the discomfort it causes during placement and removal are the main drawbacks of anterior packing with these materials. The complications brought on by anterior packing include sinusitis, syncytia, hypoxemia, arrhythmia, and septum perforation.47 In a non-randomized, controlled trial, Floseal® was found to be much more effective at stopping epistaxis than nasal packing (using Merocel, petrolatum-impregnated gauze, or Rapid Rhino) (the re-bleeding rate at 1 week was 14% vs. 40% for other treatments generally). Floseal® costs are typically high; however, they can be offset by the expense of a subsequent visit for the removal of nasal packing. The majority of doctors advise using a moisturizing saline spray for 24-48 hours after the bleeding has ceased regardless of the applied absorbable substance.48 Diseases such as arterial deterioration and HTN may be connected to this syndrome. However, posterior packing is linked to a higher risk of morbidity and mortality. Significant hypoxia may result from nasal packing, particularly in people with long-term systemic illnesses.49
Irrigation with hot water is another treatment option for epistaxis. The majority of posterior epistaxis patients are elderly, and even a brief hospital stay can increase the risk of complications and morbidity. The normal treatment for tamponade also addresses respiratory problems, including possible sleep apnea. Complications including crust development and necrosis of some nasal mucosa and ala after a few days with a firm nasal tamponade are not unusual.
The removal of blood clots from the nose, edema and narrowing of the intranasal lumen with internal and external compression of the leaking vessel, and vasodilatation of the mucosal vessels that result in a decrease in flow and intraluminal blood pressure are among the likely hemostatic effects of hot water irrigation. The clotting process could be accelerated by a rise in temperature, which is another explanation for the hemostatic effect.26
The visual analogue scale scores provided by patients who had both treatments demonstrated that hot water irrigation treatment is less painful than tamponade treatment. Throughout hot water irrigation, all these patients reported feeling less discomfort than they did during the tamponade treatment. The nasal mucosa is also extremely less traumatized by hot water irrigation treatment than by tamponade treatment.26
The success percentage of angiographic embolization for posterior epistaxis ranged from 79% to 96% when it was first published in 1974.50,51 With contrast injection comes a 4% chance of serious consequences such as a stroke, facial palsy, blindness, or nephritis. A hematoma is one of a few minor problems that happens in 10% of instances. In most circumstances, there is an 80%-90% success rate. The ligation procedure can be completed in 30-60 minutes with the use of contemporary endoscopic procedures. Despite requiring general anesthesia, endoscopic sphenopalatine artery ligation reduces the hazards of angiography. When posterior epistaxis is treated with posterior packing for immediate control and endoscopic sphenopalatine artery closure, overall healthcare costs are lowered by more than 50%.52 Sphenopalatine artery intranasal packing to stop bleeding was found to be 98% successful in 127 patients. In the aforementioned trial, no notable side effects were noted with regard to the medication.53
The application of endoscopic packing, compared to the employment of conventional posterior nasal packing, led to the lesser hospital stay. Regarding the increased risk of the internal carotid artery, or ophthalmic artery cannulation, and consequently increment the risk of stroke or blindness, the embolization of anterior and posterior ethmoid arteries is rarely performed.20 However, the risk of stroke and blindness is greatly reduced by utilizing bipolar cautery or intra-orbital vein clipping before exiting the anterior and posterior ethmoid foramen, and the external ligation of the anterior and posterior ethmoid arteries through a small incision near the middle eyebrow. Routine care of the nasal mucosa such as moisturizing the mucosa is recommended after controlling the epistaxis to prevent recurrence. Furthermore, antiseptic cream was accompanied by a reduced recurrence rate of epistaxis compared to no treatment in a randomized controlled trial. However, in terms of three different strategies (i.e., topical antiseptic cream, silver nitrate cautery, and no treatment) no difference was observed in the outcomes. Another used agent in controlling epistaxis in different included studies in the current systematic review and meta-analysis was tranexamic acid as an anti-fibrinolytic agent, with a competitive inhibitor of plasminogen activation and a non-competitive inhibitor of plasmin at low and high concentrations. Tranexamic acid inhibits the binding of plasminogen to fibrin, thereby preventing clot breakdown.12,13,28
There is no standard classification for the severity of bleeding, and it may vary from patient to patient. Specific treatment depends on the involved artery, and the correct identification of the bleeding artery is the most basic measure for an effective treatment. Differences in recurrence rates observed among different treatment methods may be due to actual differences in efficacy or differences in treatment selection by emergency department physicians based on epistaxis severity. However, cauterization with silver nitrate offers another advantage that does not need to be pursued.
Study Limitations
After reviewing studies, the heterogeneity value was obtained, indicating the existence of serious heterogeneity in the studies. Further studies are needed to clarify the most effective treatment method based on epistaxis severity.
Conclusion
The most used approach to control epistaxis was tranexamic acid, whether oral, topical, or nasal compression. Among other treatment methods, rapid rocket nasal tampon and nasal packing with Vaseline gauze had similar effects compared to placebo. The highest rate of success was related to topical tranexamic acid compared to topical oxymetazoline spray and then nasal compression with tranexamic acid compared to placebo. On the contrary, the lowest success rate was observed in the treatment with the Floseal® homeostatic agent in comparison to nasal packing, as well as in the treatment with nasal compression with tranexamic acid compared to nasal packing. Moreover, the success rate of treatment with pneumatic tamponade was low compared to choanal balloon tamponade. It seems that tranexamic acid has beneficial effects on controlling epistaxis in the elderly. However, well-designed large randomized controlled trials are necessary for accurate conclusions.
Ethics statement
The regional ethics committee of Tabriz University of Medical Sciences approved the proposal (IR.TBZMED.REC.1400.033).
Disclosure of funding source
This study is supported by research vice chancellor of Tabriz University of Medical Sciences.
Conflict of interests declaration
The authors declare that they have no conflicts of interest.
Acknowledgments
We would like to thank regional ethics committee for approval of this study.
Data availability statement
Not applicable.
Consent for publication
Not applicable
Supplementary files
Supplementary file 1. Search Strategy
(pdf)
Supplementary file 2. Data Extraction Table
(pdf)
Supplementary file 3. Data Included in the Meta-analysis
(pdf)
References
- Chu YH, Lee JC. Images in clinical medicine Unilateral epistaxis. N Engl J Med 2009; 361(9):e14. doi: 10.1056/NEJMicm0807268 [Crossref] [ Google Scholar]
- Akinpelu OV, Amusa YB, Eziyi JA, Nwawolo CC. A retrospective analysis of aetiology and management of epistaxis in a south-western Nigerian teaching hospital. West Afr J Med 2009; 28(3):165-8. doi: 10.4314/wajm.v28i3.48443 [Crossref] [ Google Scholar]
- Small M, Murray JA, Maran AG. A study of patients with epistaxis requiring admission to hospital. Health Bull (Edinb) 1982; 40(1):20-9. [ Google Scholar]
- Walker TW, Macfarlane TV, McGarry GW. The epidemiology and chronobiology of epistaxis: an investigation of Scottish hospital admissions 1995-2004. Clin Otolaryngol 2007; 32(5):361-5. doi: 10.1111/j.1749-4486.2007.01530.x [Crossref] [ Google Scholar]
- Pallin DJ, Chng YM, McKay MP, Emond JA, Pelletier AJ, Camargo CA Jr. Epidemiology of epistaxis in US emergency departments, 1992 to 2001. Ann Emerg Med 2005; 46(1):77-81. doi: 10.1016/j.annemergmed.2004.12.014 [Crossref] [ Google Scholar]
- Yüksel A, Kurtaran H, Kankiliç ES, Ark N, Uğur KS, Gündüz M. Epistaxis in geriatric patients. Turk J Med Sci 2014; 44(1):133-6. doi: 10.3906/sag-1301-58 [Crossref] [ Google Scholar]
- Parajuli R. Evaluation of etiology and treatment methods for epistaxis: a review at a tertiary care hospital in central Nepal. Int J Otolaryngol 2015; 2015:283854. doi: 10.1155/2015/283854 [Crossref] [ Google Scholar]
- Krulewitz NA, Fix ML. Epistaxis. Emerg Med Clin North Am 2019; 37(1):29-39. doi: 10.1016/j.emc.2018.09.005 [Crossref] [ Google Scholar]
- Zhou AH, Chung SY, Sylvester MJ, Zaki M, Svider PS, Hsueh WD. To pack or not to pack: inpatient management of epistaxis in the elderly. Am J Rhinol Allergy 2018; 32(6):539-45. doi: 10.1177/1945892418801259 [Crossref] [ Google Scholar]
- Schlosser RJ. Clinical practice Epistaxis. N Engl J Med 2009; 360(8):784-9. doi: 10.1056/NEJMcp0807078 [Crossref] [ Google Scholar]
- Acharya PP. Recurrent epistaxis and integrated nursing management: a case report. ORL Head Neck Nurs 2004; 22(3):12-7. [ Google Scholar]
- Akkan S, Çorbacıoğlu Ş K, Aytar H, Emektar E, Dağar S, Çevik Y. Evaluating effectiveness of nasal compression with tranexamic acid compared with simple nasal compression and Merocel packing: a randomized controlled trial. Ann Emerg Med 2019; 74(1):72-8. doi: 10.1016/j.annemergmed.2019.03.030 [Crossref] [ Google Scholar]
- Birmingham AR, Mah ND, Ran R, Hansen M. Topical tranexamic acid for the treatment of acute epistaxis in the emergency department. Am J Emerg Med 2018; 36(7):1242-5. doi: 10.1016/j.ajem.2018.03.039 [Crossref] [ Google Scholar]
- Byard RW. Lethal epistaxis. J Forensic Sci 2016; 61(5):1244-9. doi: 10.1111/1556-4029.13119 [Crossref] [ Google Scholar]
- Eberle ML, Schechter-Perkins EM, Altawil Z. Topical tranexamic acid (TXA) for the management of a bleeding arteriovenous fistula. Am J Emerg Med 2020;38(2):407.e5-407.e6. 10.1016/j.ajem.2019.158441.
- Evans AS, Young D, Adamson R. Is the nasal tampon a suitable treatment for epistaxis in Accident & Emergency? A comparison of outcomes for ENT and A&E packed patients. J Laryngol Otol 2004; 118(1):12-4. doi: 10.1258/002221504322731556 [Crossref] [ Google Scholar]
- Gudziol V, Mewes T, Mann WJ. Rapid Rhino: a new pneumatic nasal tamponade for posterior epistaxis. Otolaryngol Head Neck Surg 2005; 132(1):152-5. doi: 10.1016/j.otohns.2004.04.005 [Crossref] [ Google Scholar]
- Khan MK, Reda El Badawey M, Powell J, Idris M. The utility of FloSeal haemostatic agent in the management of epistaxis. J Laryngol Otol 2015; 129(4):353-7. doi: 10.1017/s0022215115000663 [Crossref] [ Google Scholar]
- Klossek JM, Dufour X, de Montreuil CB, Fontanel JP, Peynègre R, Reyt E. Epistaxis and its management: an observational pilot study carried out in 23 hospital centres in France. Rhinology 2006; 44(2):151-5. [ Google Scholar]
- Le A, Thavorn K, Lasso A, Kilty SJ. Economic evaluation of FloSeal compared to nasal packing for the management of anterior epistaxis. Laryngoscope 2018; 128(8):1778-82. doi: 10.1002/lary.27081 [Crossref] [ Google Scholar]
- Mattoo O, Yousuf A, Mir A, Muzaffar R, Pampori R. Control of anterior epistaxis: a comparative analysis of the decongestive effect of xylometazoline and adrenaline in idiopathic epistaxis in emergency settings. Clin Rhinol 2011; 4(3):130-5. doi: 10.5005/jp-journals-10013-1092 [Crossref] [ Google Scholar]
- Newton E, Lasso A, Petrcich W, Kilty SJ. An outcomes analysis of anterior epistaxis management in the emergency department. J Otolaryngol Head Neck Surg 2016; 45:24. doi: 10.1186/s40463-016-0138-2 [Crossref] [ Google Scholar]
- Reuben A, Appelboam A, Stevens KN, Vickery J, Ewings P, Ingram W. the use of tranexamic acid to reduce the need for nasal packing in epistaxis (NoPAC): randomized controlled trial. Ann Emerg Med 2021; 77(6):631-40. doi: 10.1016/j.annemergmed.2020.12.013 [Crossref] [ Google Scholar]
- Schlegel-Wagner C, Siekmann U, Linder T. Non-invasive treatment of intractable posterior epistaxis with hot-water irrigation. Rhinology 2006; 44(1):90-3. [ Google Scholar]
- Singer AJ, Blanda M, Cronin K, LoGiudice-Khwaja M, Gulla J, Bradshaw J. Comparison of nasal tampons for the treatment of epistaxis in the emergency department: a randomized controlled trial. Ann Emerg Med 2005; 45(2):134-9. doi: 10.1016/j.annemergmed.2004.10.002 [Crossref] [ Google Scholar]
- Stangerup SE, Dommerby H, Siim C, Kemp L, Stage J. New modification of hot-water irrigation in the treatment of posterior epistaxis. Arch Otolaryngol Head Neck Surg 1999; 125(6):686-90. doi: 10.1001/archotol.125.6.686 [Crossref] [ Google Scholar]
- Te Grotenhuis R, van Grunsven PM, Heutz W, Tan E. Use of hemostatic nasal plugs in emergency medical services in the Netherlands: a prospective study of 33 cases. Prehosp Emerg Care 2018; 22(1):91-8. doi: 10.1080/10903127.2017.1335816 [Crossref] [ Google Scholar]
- Utkewicz MD, Brunetti L, Awad NI. Epistaxis complicated by rivaroxaban managed with topical tranexamic acid. Am J Emerg Med 2015;33(9):1329.e5-1329.e7. 10.1016/j.ajem.2015.02.049.
- Van Wyk FC, Massey S, Worley G, Brady S. Do all epistaxis patients with a nasal pack need admission? A retrospective study of 116 patients managed in accident and emergency according to a peer reviewed protocol. J Laryngol Otol 2007; 121(3):222-7. doi: 10.1017/s0022215106003148 [Crossref] [ Google Scholar]
- Viducich RA, Blanda MP, Gerson LW. Posterior epistaxis: clinical features and acute complications. Ann Emerg Med 1995; 25(5):592-6. doi: 10.1016/s0196-0644(95)70169-9 [Crossref] [ Google Scholar]
- Wakelam OC, Dimitriadis PA, Stephens J. The use of FloSeal haemostatic sealant in the management of epistaxis: a prospective clinical study and literature review. Ann R Coll Surg Engl 2017; 99(1):28-30. doi: 10.1308/rcsbull.2017.28 [Crossref] [ Google Scholar]
- White A, O’Reilly BF. Oral tranexamic acid in the management of epistaxis. Clin Otolaryngol Allied Sci 1988; 13(1):11-6. doi: 10.1111/j.1365-2273.1988.tb00275.x [Crossref] [ Google Scholar]
- Whitworth K, Johnson J, Wisniewski S, Schrader M. Comparative effectiveness of topically administered tranexamic acid versus topical oxymetazoline spray for achieving hemostasis in epistaxis. J Emerg Med 2020; 58(2):211-6. doi: 10.1016/j.jemermed.2019.11.038 [Crossref] [ Google Scholar]
- Zhang Z, Zhang J, Zhang T, Yuan B, Jiang M. Expansion sponge versus vaseline gauze nasal packing in the treatment of nasal bleeding: a randomized comparative trial. Journal of Clinical Rehabilitative Tissue Engineering Research 2008; 12(19):3729-31. [ Google Scholar]
- Côrte FC, Orfao T, Dias CC, Moura CP, Santos M. Risk factors for the occurrence of epistaxis: Prospective study. Auris Nasus Larynx 2018; 45(3):471-5. doi: 10.1016/j.anl.2017.07.021 [Crossref] [ Google Scholar]
- Liao Z, Guo J, Mi J, Liao W, Chen S, Huang Y. Analysis of bleeding site to identify associated risk factors of intractable epistaxis. Ther Clin Risk Manag 2021; 17:817-22. doi: 10.2147/tcrm.s301706 [Crossref] [ Google Scholar]
- Seidel DU, Jacob L, Kostev K, Sesterhenn AM. Risk factors for epistaxis in patients followed in general practices in Germany. Rhinology 2017; 55(4):312-8. doi: 10.4193/Rhin17.105 [Crossref] [ Google Scholar]
- Min HJ, Kang H, Choi GJ, Kim KS. Association between Hypertension and epistaxis: systematic review and meta-analysis. Otolaryngol Head Neck Surg 2017; 157(6):921-7. doi: 10.1177/0194599817721445 [Crossref] [ Google Scholar]
- Sarhan NA, Algamal AM. Relationship between epistaxis and hypertension: a cause and effect or coincidence?. J Saudi Heart Assoc 2015; 27(2):79-84. doi: 10.1016/j.jsha.2014.09.002 [Crossref] [ Google Scholar]
- Lubianca-Neto JF, Bredemeier M, Carvalhal EF, Arruda CA, Estrella E, Pletsch A. A study of the association between epistaxis and the severity of hypertension. Am J Rhinol 1998; 12(4):269-72. doi: 10.2500/105065898781389985 [Crossref] [ Google Scholar]
- Waddell AN, Patel SK, Toma AG, Maw AR. Intranasal steroid sprays in the treatment of rhinitis: is one better than another?. J Laryngol Otol 2003; 117(11):843-5. doi: 10.1258/002221503322542818 [Crossref] [ Google Scholar]
- Dokuyucu R, Gokce H, Sahan M, Sefil F, Tas ZA, Tutuk O. Systemic side effects of locally used oxymetazoline. Int J Clin Exp Med 2015; 8(2):2674-8. [ Google Scholar]
- Beck R, Sorge M, Schneider A, Dietz A. Current approaches to epistaxis treatment in primary and secondary care. Dtsch Arztebl Int 2018; 115(1-2):12-22. doi: 10.3238/arztebl.2018.0012 [Crossref] [ Google Scholar]
- McLeod RWJ, Price A, Williams RJ, Smith ME, Smith M, Owens D. Intranasal cautery for the management of adult epistaxis: systematic review. J Laryngol Otol 2017; 131(12):1056-64. doi: 10.1017/s0022215117002043 [Crossref] [ Google Scholar]
- Murray S, Mendez A, Hopkins A, El-Hakim H, Jeffery CC, Côté DWJ. Management of persistent epistaxis using FloSeal hemostatic matrix vs traditional nasal packing: a prospective randomized control trial. J Otolaryngol Head Neck Surg 2018; 47(1):3. doi: 10.1186/s40463-017-0248-5 [Crossref] [ Google Scholar]
- Massey CJ, Suh JD, Tessema B, Gray ST, Singh A. Biomaterials in rhinology. Otolaryngol Head Neck Surg 2016; 154(4):606-17. doi: 10.1177/0194599815627782 [Crossref] [ Google Scholar]
- Dutta S, Mukherjee A, Saha J, Biswas G, Haldar D, Sen I. Modified technique of anterior nasal packing: a comparative study report. Indian J Otolaryngol Head Neck Surg 2012; 64(4):341-5. doi: 10.1007/s12070-011-0343-2 [Crossref] [ Google Scholar]
- Badran K, Malik TH, Belloso A, Timms MS. Randomized controlled trial comparing Merocel and RapidRhino packing in the management of anterior epistaxis. Clin Otolaryngol 2005; 30(4):333-7. doi: 10.1111/j.1365-2273.2005.01019.x [Crossref] [ Google Scholar]
- Leadon M, Hohman MH. Posterior epistaxis nasal pack. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022.
- Sokoloff J, Wickbom I, McDonald D, Brahme F, Goergen TC, Goldberger LE. Therapeutic percutaneous embolization in intractable epistaxis. Radiology 1974; 111(2):285-7. doi: 10.1148/111.2.285 [Crossref] [ Google Scholar]
- Robinson AE, McAuliffe W, Phillips TJ, Phatouros CC, Singh TP. Embolization for the treatment of intractable epistaxis: 12 month outcomes in a two centre case series. Br J Radiol 2017; 90(1080):20170472. doi: 10.1259/bjr.20170472 [Crossref] [ Google Scholar]
- McClurg SW, Carrau R. Endoscopic management of posterior epistaxis: a review. Acta Otorhinolaryngol Ital 2014; 34(1):1-8. [ Google Scholar]
- Kumar S, Shetty A, Rockey J, Nilssen E. Contemporary surgical treatment of epistaxis. What is the evidence for sphenopalatine artery ligation? Clin Otolaryngol Allied Sci 2003; 28(4):360-3. doi: 10.1046/j.1365-2273.2003.00724.x [Crossref] [ Google Scholar]